Purpose
Interventional oncology represents a new frontier in cancer treatment. Interventional radiotherapy (IRT) has the potential to improve treatment outcomes using minimally invasive procedures. Such techniques are also particularly indicated to treat elderly or frail patients [1, 2].
Interventional radiotherapy (brachytherapy and intra-operative radiotherapy), alone or in combination with other treatments (e.g., external beam radiotherapy, surgery, chemotherapy, hyperthermia, etc.), represents an option to deliver high radiation dose to a well-defined target, with acceptable dose to normal tissues.
For this reason, in view of ever-increasing number of IRT units, it might prove pivotal to investigate IRT teams’ structure, trying to understand what kind of professionals are involved, and the level of competence required, according to each professional profile.
The evidence that interventional oncology centers have a relevant role in patients’ care management as well as in clinical research, leads to the need to evaluate a specific staff education process. Over the last two decades, radiation therapy technologist (RTT) have increased their competencies and skills to manage technological upgrade, high-performance, customized techniques, and evolution of information technology [1-3].
At the same time, in order to acquire new skills and competencies, RTT training evolved, but a better practical and theorical formation in the IRT’s procedure may still be warranted. In Italy, RTTs receive their bachelor’s degree after a three-year university course in diagnostic imaging, radiotherapy, and nuclear medicine. Subsequently, RTTs are allowed to work as radiographers or radiation technologists in diagnostic radiology, nuclear medicine, and radiotherapy as well as in IRT units.
The aim of this paper was to outline a general framework of RTT role in IRT units, with a special focus on brachytherapy, to understand current professional practice and focus on the development of an IRT multi-professional team. In this contest, to better understand the level of education and training of RTTs, we considered European core curriculum by the European Society for Radiotherapy and Oncology (ESTRO) [1].
Material and methods
A 16-question survey was developed by the Italian Association of Radiation Therapy and Medical Physics Technologist (AITRO) and the Italian Association of Radiotherapy and Clinical Oncology (AIRO), using SurveyMonkey online platform (www.surveymonkey.com). The Group sent the survey through an AITRO contact list of RTTs belonging to different Italian radiotherapy centers. The survey was available online for four weeks. Answering all questions was mandatory to avoid incomplete or partial data. The Group divided the survey into three different sections, summarized as follows:
Section 1: Basic information (questions 1-3)
Hospital affiliation and type of management: for i.e., public hospital (belonging to the national health service), accredited private hospital (providing health services on the behalf of national health service), private hospital or university hospital.
Section 2: Role of RTT in IRT units (questions 4-9)
The aim of this section was to clarify the role of RTT in IRT multi-professional teams, focusing on involvement in procedures and training required.
Section 3: Background information on IRT team and type of work (questions 10-16)
Questions were defined to provide information on the team organization, health professionals involved, and types of performed brachytherapy treatments. Full questionnaire is presented in Table 1.
Table 1
Survey questionnaire
Results
A total of 37 out of 105 (36%) RTTs of Italian radiation oncology centers completed the online survey and replied to questionnaires over a one-month period. The results were as follows:
Section 1: Basic information (1-3)
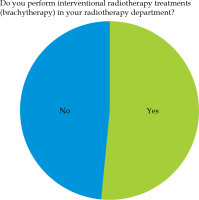
The responses received represented 65% of Italian regions (question No. 1). The majority of RTTs started to work in non-university public hospitals (35.14%) or Institute for Cancer Treatment and Research (Istituti di Ricovero e Cura a Carattere Scientifico – IRCCS) university hospitals (40.54%) (question No. 2). More than 50% of RTTs worked in hospitals, where IRT intended as brachytherapy, was performed (question No. 3; Figure 1).
Section 2: Role of RTT in IRT units (4-9)
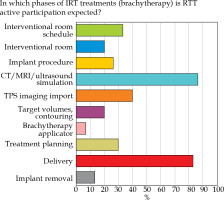
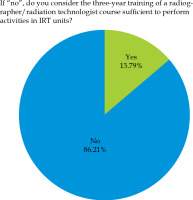
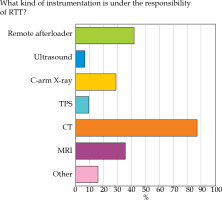
Almost 50% of the responses involved dedicated RTT staff for IRT, with active participation in all treatment phases (question No. 4; Figure 2). RTTs were mainly involved in computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound imaging (US) procedures (86.7%) as well as treatment delivery phase (83.3%), image management (40.0%), and patients’ schedule monitoring (33.3%). The number of RTTs assigned to IRT service varied from 1 (40.9%) to more than 3 (18.18%) (question No. 6). The instrumentation under RTT responsibility was mostly represented by CT (87.1%), remote afterloader (41.9%), MRI (35.5%), and C-arm X-ray systems (29.0%), respectively (question No. 7; Figure 3). 61.3% of RTT staff assigned to IRT units did not receive a specific training on site in hospitals, while 86.2% of the respondents suggested that undergraduate training may not be sufficient to work in IRT (question No. 9; Figure 4).
Fig. 3
Question No. 7 results
TPS – treatment planning system; C-arm – C-Arm X-ray system; MRI – magnetic resonance imaging
Section 3: Background information on IRT team and type of work (10-16)
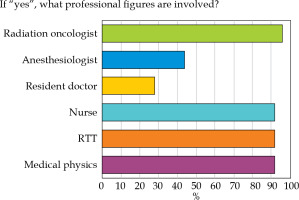
74.2% of the respondents worked in a dedicated team for IRT treatments (question No. 10). The most common professions in IRT were radiation oncologist (96%), RTT (92%), nurse (90%), and medical physicist (92%) (question No. 11). Anesthesiologists and RT resident doctors engaged in IRT teams in 44% and 28% of cases, respectively (question No. 11; Figure 5).
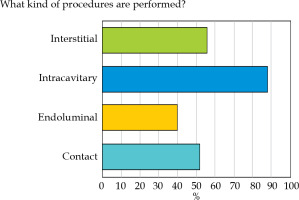
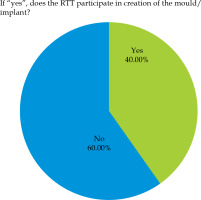
The techniques used in brachytherapy services included high-dose-rate (HDR) (69.2%), low-dose-rate (LDR) (42.3%), and pulsed-dose-rate (PDR) IRTs (15.4%) (question No. 12). As shown in Figure 6, the most frequently performed procedures involved intracavitary IRT (88%), followed by interstitial IRT (56%), contact IRT (52%), and endoluminal IRT (40%, question No. 13). 64.71% of responses indicated contact IRT, with RTT involvement in moulds preparation at 40% (question No. 15; Figure 7). Applicators used during the different procedures were managed by RTTs in 45% of cases.
Discussion
The present study promoted a national survey to investigate health professionals’ management in IRT teams in Italian radiation oncology centers. The main limitation of this survey was that one third of the referent RTTs only answered the questionnaire; therefore, the results are not likely to represent complexity of the Italian reality. The reason of a low response rate could be due to a limited number of Italian radiation oncology centers offering IRT, as revealed by the most recent national census (October 2017), which shows that in Italy, there are 195 centers (AIRO site: https://www.radioterapiaitalia.it/i-centri-in-italia/) with only 69 IRT treatment devices.
Additional reasons could be the lack of established role of RTTs in some centers and the fact that the survey was sent during first phase of the SARS-CoV-2 pandemic in Italy.
This study represents just a view of the activity of IRT units in Italy, and can be used to promote future initiatives, which could lead to a new and greater involvement of RTT personnel in IRT centers.
The evolution of professional education of RTTs in Italy came to a complete definition in the year 2000, with a recognition of bachelor’s degree as well as a decree of 3rd November 1999, No. 509, after almost twenty years of gradual legal and education development.
At the end of the three-year degree, new regulation also define a further course of training as a master’s degree, which provides advanced training for highly qualified professional activities.
Unlike other European university programs, the Italian three-year degree for RTT is not specific to radiotherapy. For this reason, RTTs working in radio-oncology departments often have to seek specific skills related to the best practices of radiotherapy administration, especially the most modern technologies [5, 6].
To recognize specific training standards, the RTT committee of ESTRO in 2001 has developed a core curriculum [4], now in its’ third edition, facilitating the development of local and national programs to optimize the existing programs of study and to identify core competencies [1].
The ESTRO Core Curriculum was based on a European survey administered in 28 countries, with the main aim to investigate the heterogeneity of training pathways among different countries and RTTs contributions to daily practice. Further documents were also published to strengthen the development of radiation therapy-specific curricula for RTTs engaging in postgraduate education, and focusing on skills and competences required to work in advanced level RT departments [5]. Other sources include the European Federation of Radiographers Societies (EFRS) European Qualifications Framework (EQF) 6 document, in which the authors underline basic competencies to perform RTT in brachytherapy [6].
In general, is it known that RTTs experiences are mostly related to positioning and immobilization, image acquisition and virtual simulation, treatment planning, treatment delivery, and quality assurance (QA).
With regard to treatment planning, ESTRO document highlights that all RTTs should be able to interpret a treatment plan, compare it with a treatment prescription, and participate in preliminary discussion on issues related to the best treatment plan of an individual patient.
Radiation therapy technologists should have dedicated knowledge for routine quality assurance of treatment equipment in IRT departments. They are responsible for ensuring the highest quality of all procedures they are involved, including safety controls before the start of treatment according to a department protocol [1-3, 5].
According to the responses of ESTRO survey [1], RTTs participate in room preparation and simulation procedures in 20 countries. Moreover, RTTs are engaged in a preparation phase of a procedure (16 countries) and in the assistance to a procedure itself (17 countries). In 12 and 10 countries, RTTs are involved in treatment planning and dose calculation, respectively [1].
These data partly overlap with the results of the survey designed for this study, especially concerning data related to simulation procedures and daily activity planning (Table 2).
Table 2
Comparison between ESTRO survey and AIRO-AITRO survey
From the results of our survey, it appears that RTTs exercise their professional role in different treatment IRT modalities. In addition to the above-mentioned phases, RTTs collaborate with radiation oncologist and nurses in room preparation and assist during implantation of different procedures, often managing the applicators. Examples of this are the best-known endocavitary and interstitial procedures in gynecological and prostate cancers.
In particular, the role of RTTs appears to be of primary importance in moulds preparation for skin tumors treated with contact IRT. Moreover, RTTs are crucial in procedure planning phase and in managing of patients’ appointments, optimizing timetable of operating rooms based on the real-time of execution of the implants, CT, treatment plan, and delivery.
In selected cases, it is suggested to consider RTT’s presence in operating rooms to collaborate with medical and nursing staff in phases of insertion and removal of the applicators (e.g., eye’s plaques, interstitial needles, or catheters).
Given the importance of a proper planning, there is a need to identify a slot to be dedicated to each individual IRT procedure. It would be optimal to divide the planning phase in two parts: the first to provide a multi-disciplinary board for discussion of clinical cases enrolled into brachytherapy, and the second part to ensure a multi-professional board, consisted of dedicated team (radiation oncologist, medical physicist, RTT, and nurse), necessary to better plan admissions, outpatient services, diagnostic tests, and procedures.
To complete, it should be emphasized that a well-structured planning could also facilitate the organization of all those operative units where IORT is performed. In IORT treatments, RTTs are responsible for technical procedure, correct functioning of all equipment, and quality control according to defined and shared protocols. Collaborating with nursing staff, whenever present, RTTs plan and manage patient paths, environmental aspects of cleanliness and sterility, and patients’ handling (no linac-based dedicated unit). RTTs also collaborate with radiation oncologists in IORT (position of the patient, movement of the couch, and equipment in relation to the position of applicator), performing irradiation along with radiation oncologists and medical physicists [7].
In any IRT technique, it is essential to understand and evaluate the roles of radiation oncologists physicists, RTTs, nurses, and other healthcare professionals to pursue patients’ care improvement and treatment delivery as well as constantly encourage working team and overlapping responsibilities negotiation [8-10].
A multi-disciplinary, multi-professional approach is needed for the best IRT treatment delivery due to complexity of the treatment workflow to perform high quality procedures [11]. The implementation of new technologies for personalized moulds, imaging techniques, and advanced surgical procedures are only feasible in a multi-professional context [12-14]. Diagnostic capabilities and therapeutic options can be easily discussed to ensure the best treatment for each patient. Additionally, patient-centered approach is essential to provide safe treatment, particularly for elderly or comorbid patients [15, 16]. For this reason, interventional oncology centers could have an important role in education as well as clinical research [17].
With reference to research pathways for RTT, the ESTRO Core Curriculum for RTT defines how this professionals should be able to evaluate and apply research results in their daily practice, with definition of large databases and predictive models [18, 19].
Conclusions
The results of this national survey could help define the current professional situation of RTTs in IRT units to promote future goals for organizational development and enhancements in education and practice.
Specific updates can be the key to encourage collaboration, thus increasing the added value of each profession in IRT teams in order to improve personalized and patient-centered treatments.