Purpose
Ampullary carcinoma (AC) arises within the duodenal ampullary complex [1]. AC is increasingly detected because of the widespread use of upper gastrointestinal endoscopy and CT, although it is still a rare malignant neoplasm [2]. Biliary obstruction, a common consequence of ampullary carcinoma, can cause impaired gastrointestinal and liver function, pruritus, and possibly cholangitis [3]. Therefore, the quality of life and survival outcome can be substantially affected. It is important to manage biliary obstruction in unresectable AC, especially in elderly patients. Since age and comorbidity may directly reduce the likelihood and willingness of surgery, insertion of a stent has been accepted as a main palliative procedure. Unfortunately, recurrent stent obstruction requires frequent replacement, which affects patients’ quality of life. Additionally, stenting has a limited effect on survival time [4, 5]. Another problem with AC is duodenal obstruction that also seriously impacts quality of life and survival of patients. Iodine-125 (125I) brachytherapy has been used in the treatment of malignant tumors owing to its curative effect, minimal surgical trauma, and tolerable complications [1, 6, 7]. Moreover, a multicenter study suggested that the insertion of an irradiation stent could achieve better patency and longer survival in patients with unresectable malignant biliary obstruction [8]. Several other studies have also reported that patients with malignant obstructive jaundice probably obtain varying degrees of survival benefits [4, 9, 10]. Our previous study demonstrated that 125I seed implantation was effective in unresectable pancreatic cancer [4]. However, these studies mainly focused on pancreatic cancer or cholangiocarcinoma, rather than AC. Therefore, in this study, we aimed to investigate the effects of 125I seed implantation performed under endoscopic ultrasound (EUS) in patients with unresectable AC aged at least 65 years, after relief of obstructive jaundice by stent placement via endoscopic retrograde cholangiopancreatography (ERCP).
Material and methods
Participants and study design
This was a single-center, retrospective analysis study. Data were collected from January 1, 2010 to October 31, 2020. Inclusion criteria were as follows: 1. Age 65-90 years; 2. Histopathologically confirmed AC; 3. Symptoms related to biliary obstruction, such as jaundice, pruritus, cholangitis, or pain, and need for endoscopic treatment; 4. Unresectability due to extensive lesions, metastases, comorbidity as well as refusal to surgery, external beam radiotherapy (EBRT), and chemotherapy; 5. With clear consciousness, cooperation, and the American Society of Anesthesiologists (ASA) classification performance status of 0, 1, 2, or 3.
Exclusion criteria were: 1. Carcinomas of adjacent pancreas, bile duct, or duodenum; 2. ASA performance status of 4; 3. History of bile tract surgery; 4. Active hepatitis; 5. Other primary cancers occurring within less than 5 years; 6. Expected survival of less than 3 months; 7. Bile duct stents that could not be successfully placed.
This study was approved by the Research Ethics Committee of the First Medical Center, Chinese PLA General Hospital (approval number: S2021-309-03), and complied with the Declaration of Helsinki. Written informed consent was obtained from all patients.
All enrolled cases underwent a detailed tumor examination using enhanced CT scans with 1.5 mm thickness or MRI within a week before the surgery. Then, the whole cohort received ERCP under intravenous anesthesia, which aimed to identify the stenosis of biliary and pancreatic ducts. Either a plastic stent (Cook Medical, Bloomington, IN, USA) or a fully covered self-expandable metal stent (Boston Scientific, Marlborough, MA, USA) were implanted. Distal end of the stent was placed at least 2 cm from the area of stenosis. After biliary obstruction was relieved, depending on the will of patients and their families, those who chose subsequent 125I seed implantation were entered in the treatment group, whereas the rest of patients were included in the control group.
EUS-guided 125I seed implantation
Prior to performance, in accordance with principles of Paris system, a radiologist and endoscopist in charge of the operation formulated implantation plan that included the optimal access for implantation (site, direction, and depth), prescription dose, number of seeds, single-seed activity, and seed distribution according to enhanced CT or MRI. The plan was finally tailored by the endoscopist in terms of tumor condition under EUS. Radioactivity of 125I seeds (China Isotope & Radiation Co., Ltd., Beijing, China) used in this study was 0.4 mCi (14.8 MBq). Temperature-sterilized seeds were first installed in radiation resistant metal clips into a Mick 200-TPV applicator that was later connected to a 19-gauge fine-needle aspiration needle (Cook Medical, IN, USA). Volume, morphology, and margins of the tumor, along with its relationship to surrounding tissue were assessed again under EUS in order to modify the plan. Next, the needles were inserted into the planned site (distal edge of the mass), and arranged in a general density of 5 to 10 seeds/cm under EUS (Olympus Corporation, Tokyo, Japan) guidance. To prevent seeds migration, the implant procedure was suspended when the needle moved into lateral edge of the lumen 2-3 mm. There was no overlap between each puncture track (previously implanted seeds could not be seen in the puncture field of vision). Finally, the seeds were placed in a straight line, parallel to each other, and equidistant from each other. Precautions were taken to avoid puncture of blood vessels and biliopancreatic tract during the whole process. After implantation, the position and distribution of 125I seeds in lesions were evaluated by fluoroscopy. In terms of radiation safety protection, the endoscopist and assistants were routinely wearing lead clothing, gloves, and glasses. Before being released, all 125I seeds were placed in a protective gear in special area with radiation protection. Patients and their main family members were provided with information about relative radiation protection and knowledge before and after the treatment.
Post-operative follow-up
Vital signs were monitored for at least 2 hours, and patients remained fasting for at least 12 hours after ERCP and/or 125I seed implantation. All patients (including the control group) were monitored regarding the presence or absence of procedure-related complications, and medication was administered if needed. All patients were follow-up with routine blood test and liver function at 1 week, 1 month, and then at 3-month intervals. Follow-up imaging (mainly enhanced CT scans) and endoscopy (EUS, if necessary) in the treatment group, and only imaging (abdominal CT/MRI, or ultrasound) in the control group were performed every 3 months.
In most hospitals in China, the bile stent is routinely not replaced until jaundice reappear, which is different from other countries. In the treatment group, the stents were replaced or removed according to the tumor and bile duct status at 6-month follow-up. 125I re-implantation in the treatment group depended on the tumor growth during follow-up visits. Post-procedure chemotherapy, if recommended by the oncologist and according to the patient will, was performed during follow-up. The final follow-up appointment was in July 2021.
Observed indicator and definition
The maximum intervention interval for biliary obstruction was adopted as the longest period between two adjacent palliative drainages, or from the drainage to death. Stent patency was calculated between the date of stent placement and the first episode of stent restenosis. Since the stents were routinely replaced or removed in patients in the treatment group at 6 months after the first 125I seeds implantation, the stent re-stenosis rates were only calculated at 90 days and 180 days after the first stent insertion. Stent re-stenosis was defined if patients presented clinical signs of recurrent jaundice with elevated bilirubin levels along with biliary dilation on CT, MRCP, ultrasound, or percutaneous transhepatic cholangiography [8]. Overall survival was defined as the time from stenting to death, or the last follow-up visit. Frequency of intervention was set as the overall survival divided by the number of palliative drainages. Relief of jaundice was specified as the reduction of more than 20% of total bilirubin within 1 week after stent implantation. Duodenal obstruction was described if patients presented related clinical signs along with duodenal stenosis on X-ray, CT, or endoscopy. Adverse events were analyzed after the first treatment and evaluated according to the common terminology criteria for adverse events (CTCAE v. 5.0).
Statistical analysis
Variables were presented as the numbers (percentages) or medians and interquartile range (IQR). Baseline characteristics and complications were analyzed using Kruskal-Wallis, Pearson chi-square (χ2), or Fisher exact tests. Maximum intervention interval for biliary obstruction was investigated with both Cox regressions on the cause-specific hazard ratio (HR) to show the effects of 125I seeds on control of obstructive jaundice. Censored case was defined as event-free at the time of study completion or loss to follow-up. Survival time to duodenal obstruction was analyzed using Kaplan-Meier method. Univariate analysis was performed for Cox model to identify risk factors for re-intervention of obstructive jaundice and overall survival separately. All statistical analyses were performed with R software (version 4.0.5). Two-sided tests were done, and statistical difference was indicated with p-value < 0.05.
Results
Patients characteristics
A total of 46 patients were enrolled. One patient was lost to follow-up after 125I implantation, and one died accidently two weeks after insertion of a stent. Finally, 11 patients in the treatment group and 33 patients in the control group were included in this study. Baseline characteristics showed balance between the two groups (Table 1).
Table 1
Demographic and clinical characteristics of the study groups
125I implantation in treatment
No radioactive seed-related technical failures were encountered. The median of 2 times puncture per patient was applied (range, 1-5). The median of 20 seeds (range, 15-40) was implanted per patient, with a median implanted activity of 8.0 mCi (range, 6-16) during the first treatment.
Observed indicator
The median maximum intervention interval for biliary obstruction in the control group was 175 days (IQR: 126-274 days), and in the treatment group was 381 days (IQR: 204-419 days). Patients in the 125I group were associated with a decrease in the rate of re-intervention (HR = 0.31, 95% CI: 0.14-0.71%) (Tables 2, 3, and Figure 1). The stent re-stenosis rates at 90 days and 180 days in the control group were 12.9% and 51.6%, respectively. No stent stenosis was found in the treatment group within 180 days.
Table 2
Univariate analysis for risk factors of recurrence
Table 3
Multivariate analysis for risk factors of recurrence
| Parameter | HR | 95% CI | p-value | |
|---|---|---|---|---|
| Group | ||||
| Control group | 1 | |||
| Treatment group | 0.24 | 0.10-0.57% | 0.0012 | |
| Grade | ||||
| Grade I | 1 | |||
| Grade III | 2.13 | 0.80-5.65% | 0.1293 | |
| Grade IV | 3.34 | 1.55-7.23% | 0.0022 | |
Fig. 1
Cumulative hazard from Cox model (HR = 0.31, p = 0.006, 95% CI: 0.14-0.71%). Figure supports that group type was associated with a decrease in rate of re-stenosis
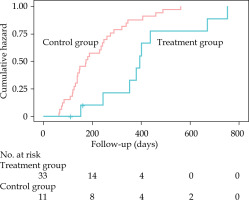
Re-intervention was performed in 35 of 44 patients (9 in the treatment group and 26 in the control group) who experienced stent re-stenosis. Twenty-eight patients (9 in the treatment group and 19 in the control group) underwent additional stent implantation, and 7 patients in the control group underwent percutaneous transhepatic biliary drainage (PTBD). In the other 8 patients (1 in the treatment group and 7 in the control group), re-intervention was not attempted due to poor systemic conditions, limited life expectancy after re-intervention, patient refusal, or other reasons. Stent re-stenosis was not observed in patients in the treatment group in the whole follow-up time.
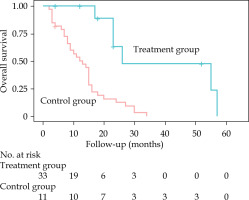
During the median follow-up of 15 months (IQR: 7.75-23 months), 6 (13.64%) patients were alive and 38 (86.36%) patients died. The causes of deaths included cancer cachexia (42.42%), multiple organ dysfunction syndrome (MODS; 34.21%), severe infection (21.05%), tumor-associated hemorrhage (5.26%), unknown (2.63%), etc. The median survival was longer in the treatment group than that in the control group (26 months and 13 months, respectively; p < 0.01, Figure 2). In the overall survival, patients in the treatment group accepted more interventions for biliary obstruction (3 vs. 2). The median frequencies of intervention for palliative drainage were 7.67 vs. 6 months (IQR: 6.00-15.16 vs. 3.5-7.5 months) in the treatment and control groups, respectively.
Fig. 2
Overall survival from stent implantation. Overall survival in the treatment group was longer than that in the control group (HR = 0.24, p = 0.0012, 95% CI: 0.10-0.57%)
The relief of jaundice within one week after stent placement was recorded in 81.82% (2/11) of patients in the treatment group and 84.85% (5/33) in the control group (p > 0.05). Other symptoms associated with biliary obstruction (pruritus, cholangitis, pain, etc.) were relieved at various degrees after stent implantation.
There was no difference between the rates of duodenal obstruction recurrence in the two groups (54.54% and 60.61% in the treatment and control groups, respectively, p > 0.05); however, the median time to recurrence of duodenal obstruction was longer for the patients undergoing seed implantation than for the control patients (20.5 and 11 months; IQR: 15.75-49.25 and 6.25-14.75 months, respectively; p < 0.05).
There was no procedure-related mortality in this study. The overall incidence of adverse events was comparable (36.36% in the treatment group and 27.27% in the control group; p = 0.706). Abdominal pain was the most common complication, with 27.27% in the treatment group and 12.12% in the control group (Table 4). All of these problems were alleviated with symptomatic treatment, followed by two adverse events of grade 3 (CTCAE version 5.0, including one pancreatitis and one cholangitis, 6.06%) in the control group, and all patients recovered with conservative management.
Table 4
Adverse events
Discussion
Ampullary carcinoma is a rare malignant neoplasm without established optimal protocols for inoperable patients. Similar to pancreatic head adenocarcinomas and distal cholangiocarcinomas, obstructive jaundice is a common manifestation of ampullary cancer (up to 80%) [11]. As a palliative management for decompression of malignant biliary obstruction, stent implantation under endoscopy is extremely effective in providing symptomatic relief and improving patient quality of life [12], while stent patency remains a complicated challenge. Cholangitis due to stent restenosis, exacerbates frailty and comorbidities in the elderly, which finally promotes mortality. Researchers have been attempting to improve stents to enhance patency rates and delay re-stenosis. However, the problem is still not well-solved. Compared with plastic stents, metal stents have longer patency, but a risk of bleeding. Also, tumor development through the mesh or overgrowing at both ends of the stent have been main limitations of uncovered self-expandable metal stents [13]; covered metal stents are also prone to shifting and falling off. In addition, stent implantation alone has a limited effect on survival time [5]. 125I seeds implantation has rapidly increased in treating many solid tumors with acceptable toxicity, and has been certified as a standard of treatment in prostatic cancer [7, 14]. Intra-luminal brachytherapy, with 125I seeds strands and 125I seed-loaded biliary stents, has been applied to the treatment of malignant biliary obstruction, providing longer stent patency and better survival compared with stent placement alone [8, 10]. However, in the management of AC, an irradiation stent might not be as suitable, since the seeds in the stent cannot be distributed effectively and evenly in AC tumor, which might even impair adjacent normal bile ducts. In addition, brachytherapy of 125I seed-loaded irradiation stent is effective for about six months, and patients cannot receive re-implantation of new 125I seeds to maintain brachytherapy. Nevertheless, radioactive stents cannot restore the seed implantation source. In contrast, the biliary stenting combined with the implantation of 125I seed shows an obvious superiority in the replacement of 125I seeds when appropriate [15].
Furthermore, frequent interventions affect patients’ quality of life. Overall survival of ampullary carcinoma is longer than that of other periampullary carcinoma. Therefore, AC patients with biliary obstruction face more frequent interventions. In this study, the combined treatment of endoscopic biliary stenting with 125I seeds implantation in unresectable AC was applied. The median maximum intervention interval for palliative drainage in the treatment group was 381 days compared with 175 days in the control group. The median frequency of intervention in the treatment group was superior then in the control group (7.67 and 6 months). Also, there was no stent re-stenosis in the treatment group compared with 12.9% and 51.6% in the control group at 90 and 180 days, which suggest that the stent patency in the treatment group was better than that in the control group.
The median maximum intervention interval of stents alone in the current study was a little longer than the results from previous studies (132.7 days with metal stent and 128.5 days with two plastic stents) [16]. This might be attributed to different baseline characteristics of included patients. Unlike the results from other studies on malignant biliary obstruction [17], the present study results showed that stent type was not a risk factor for stent stenosis in multivariate analysis, which is in line with a study on ampullary cancer [16]. Metal stents in ampullary cancer might be associated with a shorter patency compared with tumors at other sites. Park speculated that tumor growth patterns of ampullary cancer might be related to this tendency [16]. Both univariate and multivariate analyses showed that group was a risk factor in a re-intervention, suggesting that 125I seeds implantation prolongs the intervention interval. The advantage was in accordance with previous studies on application of brachytherapy in malignant biliary obstruction [8]. Another risk factor was tumor stage, which indicated that tumor progression accelerated stent stenosis. This is also consistent with clinical observations.
In the present study, the median survival in the patients who accepted 125I seeds implantation was longer than that in the control group. Group type was found to be an independent risk factor for survival, and indicated that 125I seeds implantation prolonged the survival of ampullary cancer patients. Since brachytherapy in ampullary carcinoma has not been reported before, it is difficult to directly compare our results. However, the advantage in survival was in accordance with a previous trial examining biliary tract and pancreatic carcinoma patients [4, 18]. In this trial, the median survival in the treatment group was 26 months, which was 13 months longer than survival of patients in the control group who underwent stenting alone. Moreover, the median prolonged survival was 2.3 months in our previous study on pancreatic patients and 3.15 months in a systematic review on malignant biliary obstruction (biliary tract and pancreatic carcinoma) [4, 19]. This could be due to different cancer types, indicating that patients with ampullary cancer benefit more from brachytherapy than other periampullary carcinoma cases. Additionally, the frequency of treatment may be another factor, since half-life of 125I seed is 59.4 days and approximately 90% of the energy is released in three half-lives; therefore, timely complementary treatment is critical.
Duodenal obstruction, a common but difficult problem in patients with advanced ampullary carcinoma, affects life quality and endoscopic re-intervention. Clearly, there is no reported method for reducing its incidence or delaying occurrence time. In this study, patients undergoing seed implantation demonstrated a prolonged median time to duodenal obstruction, which has not yet been reported by other investigators. This result could be due to implanted 125I seeds inhibiting the growth and invasion of tumors.
A total of 4 patients (36.36%) developed post-operative adverse events in the treatment group compared with 9 patients (27.27%) in the control group (p = 0.706). None of brachytherapy-related grade 3 or 4 adverse events occurred in the current study. These results indicate that the dosimetry of 125I seeds is well-tolerated.
This study has some limitations. First, single-center retrospective study with relatively small number of patients. Second, the study was conducted in senior patients, and the feasibility of 125I seeds implantation in younger patients warrants further investigation. Third, brachytherapy as a local treatment has its limitations, and the vast majority of patients in this study did not receive combined chemotherapy. Therefore, the effectiveness of chemotherapy in prolonging survival in the present study could not be assessed.
Conclusions
Iodine-125 seeds implantation combined with bile duct stents provides longer intervention interval for biliary obstruction, delay in duodenal obstruction, and subsequently improves the overall survival in patients with unresectable ampullary carcinoma compared with a conventional stent alone.