Introduction
To achieve not only effective weight loss, but also remission of comorbidities, various surgical methods are used in the treatment of obesity. The most common procedures performed worldwide are sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and one anastomosis gastric bypass (OAGB) [1]. Santoro et al. proposed a new method of diversion of ingested food into the ileum and the normal pathway into the duodenum [2]. They originally used Roux-en-Y anastomosis. A few years later, Mahdy et al. modified the Santoro procedure [3]. They used a single loop anastomosis between antrum and the ileum, calling it a single anastomosis sleeve-ileal bypass (SASI). The bipartition mechanism is preserved while simplifying the procedure to one anastomosis.
Several other studies have confirmed the observed efficacy and safety of SASI [4, 5] The advantage of the procedure is the access to the duodenum and the papilla, and the possible lower risk of nutrient deficiencies and malnutrition [3]. Moreover, SASI is a reversible procedure. At any time, it is possible to separate the loop from the gastric antrum. However, only a few, short-term studies and observations are available [4, 5]. Due to the small number of papers on this subject, we decided to present and analyse our results of SASI.
Aim
The aim of this study is to present the results of the first group of patients from a bariatric centre in central Europe. The second aim is to compare SASI as a primary and revisional procedure.
Material and methods
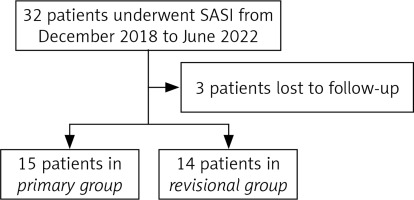
This was a retrospective cohort study. We analysed patients who underwent SASI for obesity in one bariatric department from December 2018 to June 2022 by the same team of surgeons. Patients were qualified for surgery according to national and international criteria. All patients gave appropriate consent to perform the procedure. There were 2 groups of patients. The first group consisted of patients who underwent SASI as their first bariatric and metabolic procedure (primary group – PG). The second group consisted of patients who underwent SASI after previous SG procedure due to weight regain and/or symptoms of gastroesophageal reflux disease (GERD) (revisional group – RG). From the RG we specified RG-WR for a patient who was reoperated because of weight regain. Preoperative gastroscopy was performed in all patients. Confirmation of GERD was established by Los Angeles C or D, or Barret’s oesophagus according to the Lyon consensus [6]. In RG patients without GERD on gastroscopy but with subjective GERD symptoms had 24-hour impedance pH monitoring. Postoperative gastroscopy and 24-hour impedance pH monitoring was performed in patients suffering from GERD. The postoperative survey was performed during personal or telephone consultations 6 months after the surgery and every 12 months thereafter. It included weight loss reported as a percentage of excess weight loss (%EWL) and percentage of total weight loss (%TWL). Patients were also questioned about comorbidities: type 2 diabetes (T2D), hypertension (HT), and their remission, and the presence of GERD. All outcomes are reported according to standardized outcomes reporting by the American Society for Metabolic and Bariatric Surgery (ASMBS) [7]. We also analysed the length of hospital stay (LOS) expressed in days after surgery, operative time, and complications throughout the follow-up. Patients who did not appear for subsequent follow-up visits and did not agree to participate in the study were lost to follow-up and were not analysed in the study.
Surgical technique
All patients underwent SASI according to standard technique [8]. The sleeve was started 6 cm before the pylorus calibrating using a 36 French nasogastric tube. The ileal loop was measured approximately 350 cm proximally to ileocecal valve. Then a 3 cm gastro-ileal anastomosis using a linear stapler was made. The defect was closed with an absorbable self-locking suture. Routinely no drain was left.
Ethical considerations
The data were completely anonymized. The study was conducted in accordance with the ethical standards of Helsinki Declaration of 1964 and its subsequent amendments. The study was approved by the Bioethics Committee of the Regional Chamber of Physicians, District of Warmia and Mazury, Poland (3/2023/VIII). Informed consent was obtained from the participants included in the study.
Statistical analysis
Statistica, Software Inc., Krakow, Poland (2017) software was used for statistical analysis. Descriptive statistics were used. The mean and standard deviations were estimated. Student’s t-test was applied for the correlated variables. A p-value of < 0.05 was considered statistically significant.
Results
Twenty-nine patients who underwent SASI in one bariatric centre in Poland were analysed in this study. There were 15 patients (80% female) in the PG and 14 patients (88% female) in the RG. Three patients were lost to follow-up (Figure 1) – they were not included in the analysis. The follow up rate was 91%. The mean age was 40.3 ±7.6 years and 42.3 ±7.8 years, respectively. In the PG, the mean preoperative BMI was 40.1 ±4.0 kg/m2, LOS was 1 day, and the mean operating time was 84 ±25.5 min. In the RG the mean BMI was 36.6 ±8.72 kg/m2, the length of hospital stay was 1 day, and the mean operative time was 81.3 ±28.3 min. The mean follow-up time was 26.9 ±6.1 months in PG and 17.1 ±13.5 months in RG. The revisional surgeries were performed for weight regain and/or GERD. Eight patients were operated on for weight regain (RG-WG), and 8 patients for GERD. Among them, 3 patients underwent revisional bariatric surgery for both reasons. In the PG, 13 patients had T2D, 9 had HT, and 10 had GERD. While in the RG, 2 patients had T2D, 4 had HT, and 11 had GERD (Table I).
Table I
Characteristics of patients
In the PG, %EWL 6, 12, 24, and 36 months after surgery was 68.8%, 104.5%, 115.8%, and 113.9%, respectively. %TWL in the PG was 25.2%, 37.8%, 44.6%, and 43.9%, respectively, 6, 12, 24, and 36 months after surgery. In the RG, %EWL 6, 12, and 24 months after surgery was 59.5%, 59.0%, and 56.9%, respectively. In the PG, %TWL 6, 12, and 24 months after surgery were significantly higher than in the RG (p = 0.002, p < 0.001, p = 0.008, respectively) (Table II).
Table II
Outcomes of SASI in the primary group (PG) and the revisional group (RG)
Patients in the PG achieved significantly higher %EWL 6, 12, and 24 months after surgery than patients in the RG-WG (p = 0.021, p = 0.001, p = 0.004, respectively). In the PG, %TWL 6, 12, and 24 months after surgery were significantly higher than in the REDO-WG (p = 0.04, p = 0.001, p = 0.02, respectively) (Table III).
Table III
Outcomes of SASI in the primary group (PG) and the revisional group for weight regain (RG-WG)
In the PG, 12 (92.3%) patients had complete remission of T2D after surgery, and 7 (77.9%) had complete remission of HT. In the RG, all patients had complete remission of T2D and HT (2, 2 retrospectively). In the PG, 5 (50%) patients had complete or partial remission of GERD, while in the RG, 9 (81.8%) patients had remission. Worsening of GERD was reported in 4 (40%) patients in the PG (Table IV).
Table IV
Improvement in comorbidities after SASI in the primary group (PG) and the revisional group (RG)
There were no prolonged LOS or deaths in the study group. There was one 30-day Clavien-Dindo Grade III complication. One patient in the PG developed a leak 5 days after surgery. The sewing of perforation was performed with a good outcome. One case of severe bilious vomiting was observed 1 year after surgery. The patient needed reoperation, and the intestinal loop was separated with a good outcome.
Discussion
Our study is a retrospective analysis of 29 patients who underwent SASI in our department. It was shown that SASI achieves a satisfactory effect, both bariatric and metabolic, in the short- and medium-term follow-up. To our knowledge, this is one of the first papers to provide 2- and 3-year follow-up after SASI and describes SASI as a revisional procedure.
According to our study, 12 months after primary procedure, patients achieved 104% EWL (67.9–170.9%). The largest meta-analysis, by Emile et al., showed that 12 months after SASI, patients achieved approximately 90% EWL [5]. The same paper analysed the improvements in comorbidities. Between 78.5% and 100% of patients showed an improvement [5]. In our study, 92.3% had complete remission of T2D in the PG. The improvement in HT was estimated in the meta-analysis from 36.1% to 90.2%. In our study, 77.9% had complete remission of HT in the PG. Furthermore, our study met with the results of a meta-analysis in a short-term follow-up [5].
Fifty percent of patients with GERD improved after DN SASI, but up to 40% of patients reported worsening of their symptoms after SASI. The improvement rate is much lower than in other papers [5]. Differences between these studies may be due to variances in patient selection and the small number of patients who underwent SASI in the out department. Hence, further studies are needed.
Twenty-four and 36 months after surgery, the patients in the PG maintained an excellent bariatric effect. %EWL was 115.8% and 113.9%, respectively. We found only one study that showed a 3-year follow up after SASI [9]. Hosseini et al. reported that %EWL after 3 years was 80.6% [9]. The authors calculated %EWL using the same scheme as ours, but the number of patients was larger in their group, so this may be a reason for the differences.
Our study analysed both primary and revisional surgeries. To our knowledge, there are only 2 cases in the literature describing SASI as a revisional bariatric procedure [10, 11]. We performed 16 revisional SASI after SG. In 8 cases, the reason was weight regain and in 11 cases GERD. In the RG-WG 6 achieved 12-month follow-up and 4 patients achieved 24-month follow-up. %EWL was 34.4% and 24.7%, respectively. The most frequently performed revision procedures in Poland are OAGB and RYGB, and SASI may have similar results to OAGB and RYBG reported in a recent analysis [12, 13]. Moreover, 9/11 patients with GERD improved, which may be promising for revisional procedure for GERD. However, the latest Delphi consensus does not recommend SASI as a revisional procedure after SG for GERD symptoms [14]. Due to the small number of people analysed, further work is needed to assess the efficacy of SASI as a revisional surgery.
The limitations of our study are the small sample size and its retrospective character. However, due to the very small number of papers describing SASI, a relatively new procedure, this paper contains important observations.
Conclusions
The short- and medium-term effectiveness of SASI may be satisfactory. It may be an effective and safe method for the treatment of obesity. SASI may be an effective method of revisional bariatric surgery performed for GERD. However, it had poor outcomes in revisional bariatric surgery performed for weight regain.