Introduction
Endovascular aortic repair (EVAR) is nowadays a widespread method of managing abdominal aortic aneurysm (AAA). Since its introduction, the devices used to perform it have been constantly improved, so that more and more patients may be eligible for this method. New generations of stent grafts are more flexible and have smaller diameters of their insertion systems. Low-profile stent grafts (LPSGs) make it possible to treat patients with anatomically challenging aneurysms, and facilitate a percutaneous and thus less invasive procedure [1]. It is an important issue, since concomitant iliac artery stenosis is present in 36% of patients with AAA, increasing the risk for arterial injury of the access vessel at the time of EVAR [2]. The INCRAFT AAA Stent-Graft System (Cordis Corporation, Milpitas, CA, USA) is a new-generation endograft with an ultra-low-profile delivery system to facilitate access through tortuous and/or diseased iliac access vessels [3].
Aim
To compare the short term outcomes of standard-profile stent grafts (SPSGs) and INCRAFT LPSG for EVAR of AAA.
Material and methods
Setting and design
This single-center, case-matched retrospective study was performed in accordance with the Declaration of Helsinki and in line with the requirements of the local ethics committee (approval no. OIL/KBL/29/2023). Prior to the operation, all patients gave their informed consent for the procedure. The study was an investigator-driven initiative performed without any financial support from the industry.
Patients
Between May 2020 and December 2022, 31 patients with AAA were treated by EVAR using an LPSG. In this period 132 patients underwent SPSG implantation. After collection of patients’ data, we created a control group of patients treated with SPSGs, using statistical matching with MedCalc software. The clinical records and the preoperative and follow-up computed tomography (CT) angiography of patients who underwent endovascular treatment of AAA at our center were included in this study. After the initial surgery, clinical follow-up examinations were arranged for 3, 6 and 12 months. The morphologic alterations of the aneurysm and the aortic graft as well as the patency of the treated arteries were evaluated with ultrasound (USG) and CT angiography (CTA) as the most useful surveillance methods [4]. Reintervention was performed when necessary.
Operation details
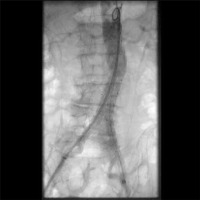
All patients in the LPSG group were treated with an INCRAFT (Cordis Corporation, Bridgewater, NJ) stent graft (Photo 1). It is a laser-cut, electropolished self-expanding nitinol stent (with fixation barbs and radiopaque markers) covered by a seamless, low-porosity polyester fabric deployed through a sheath size delivery system of as low as 14 F. We specifically opted for the INCRAFT stent graft in patients with narrow access vessels of diameter lower than 6 mm. The SPSG group was treated with different types of SPSGs (E-tegra, Artivion, Hechingen, Germany; Endurant, Medtronic Inc., Minneapolis, MN, USA) consisting of a conventional woven polyester fabric sutured to a stainless steel stent exoskeleton, delivered through a 20–22 F introducer delivery system (Photo 2). If percutaneous, femoral access was closed using a percutaneous suture device (ProGlide, Abbott Vascular Devices, Abbott Park, IL, USA), single device after 14 F systems and a double device after bigger systems.
Measured outcomes
The primary outcomes were postoperative complications and reintervention rate and 1-year mortality. Secondary outcomes were operative and postoperative parameters (additional intraoperative procedures, need for blood transfusion, postoperative morbidity, length of stay, 30-day mortality).
Statistical analysis
All data were analyzed using Statistica version 13.0 PL (StatSoft Inc., Tulsa, OK, USA); only matching was performed with MedCalc (MedCalc Software Ltd., Belgium). The results are presented as mean and SD for normal distributed data, median and interquartile range (IQR) for non-normally distributed data. The Fisher exact test was used to evaluate categorical variables. The Shapiro-Wilk test was used to check for normal distribution of data and Student’s t-test was used for normally distributed quantitative data. The Mann-Whitney U test was used for non-normally distributed quantitative variables. Statistical significance was set at p < 0.05. To identify the risk factors uni- and multivariate logistic regression was performed.
Results
Table I presents demographic characteristics of the study group. Of note, patients in the LPSG group had significantly more often low access vessel diameter (< 6 mm) compared to the SPSG group (38.7% vs. 6.7%, p = 0.003). These 2 patients with narrow vessel access had only local stenosis and required only balloon angioplasty to access the vessel with a standard stent graft system. They also had higher proximal neck diameter. Otherwise there were no significant differences between the groups in terms of demographics, comorbidities, aortic morphology and laboratory tests. Also no differences were found in perioperative and postoperative characteristics (Tables II and III). In both groups none of the patients died in the 30-day postoperative period.
Table I
Baseline patient characteristics
Table II
Perioperative characteristics
Table III
Postoperative characteristics
In 1-year follow-up, there was no rupture, no infection, no conversion to open repair and no aneurysm-related death (Table IV). Five secondary interventions were necessary in the SPSG group and only 1 in the LPSG group, although it did not reach statistical significance. The change in aneurysm sac diameter, endoleak and mortality rate did not differ between the groups.
Table IV
Follow-up characteristics
In logistic regression analysis type of stent graft was not a risk factor of perioperative complications, presence of endoleak or reintervention (Tables V–VII). Risk factors for perioperative complications were COPD and conical neck. The risk factor for endoleak was lower maximal aneurysm diameter, although the odds ratio was minimal. The risk factor for reintervention was proximal neck diameter (OR = 0.77, 95% CI: 0.6–0.97, p = 0.03).
Table V
Risk factors of perioperative complications
Table VI
Risk factors of postoperative endoleak
Table VII
Risk factors of reintervention
Discussion
Our results showed comparable results of LPSGs with normal-profile stent grafts. This issue is of utter importance since in the past years we have observed a rising amount of minimally invasive abdominal aneurysm treatment.
The overall complication rate and mortality in our study showed no difference from previous reports on the use of EVAR [5]. When compared to the group of patients treated with standard-profile devices, the 1-year clinical and radiological results of the current investigation demonstrated no increased risk of endoleak, reintervention or mortality after employing low-profile aortic stent grafts. LPSGs have some advantages over SPSGs. Previous investigations assessed the safety and efficacy of the INCRAFT stent graft but there was no comparison to SPSGs [6, 7].
In our study patients with low-profile abdominal aneurysm repair had comparable short-term results, including perioperative complications such as endoleak, to normal-profile stent grafts.
The surgical common femoral artery cutdown paradigm has gradually given way to a percutaneous-first strategy to EVAR over the past years [8, 9]. Both patients and surgeons are drawn to a completely percutaneous approach to EVAR because the smaller surgical insult is linked to a lower risk of wound complications and faster healing [8, 10]. Nevertheless, the percutaneous approach is less possible and bears more risk with higher profiles of stent graft systems [11]. In a meta-analysis of 2,257 patients the technical failure rate was significantly higher with a larger sheath size (≥ 20 F) [12]. Therefore low-profile systems are useful in making EVAR an even more minimally invasive technique.
One of the limitations of EVAR is narrowness of the access vessels – femoral and iliac arteries. If the cause is atherosclerotic stenosis, it is possible to expand it with balloon angioplasty [13]. In some patients the vessels are narrow in general as their anatomical feature. In such cases, it is generally not possible to expand iliac arteries as it carries a risk of artery rupture [14]. Inadequate access vessel size is more common in women [15]. Therefore they are less likely to meet device instructions for use (IFU) criteria and undergo EVAR, although they have almost double the operative mortality compared to men following open repair [15, 16]. Long-term survival is also reported to be greater in women [17, 18]. Moreover, women more often undergo adjunctive access procedures and experience higher rates of access complications [19]. For better preparation for the procedure, especially in terms of narrow iliac vessels, 3D printing devices can be used [20]. 3D printing is also efficient in detection of splanchnic artery aneurysms, which is a serious diagnostic problem in patients [21].
Our study has some limitations which should be noted. At first the study has a retrospective design. The number of patients is also limited, which creates obvious selection bias. Therefore we decided to design a case matching study to minimalize selection bias, although in our opinion the study would have benefited from randomization of the patients.