Purpose
Squamous cell carcinoma of the cervix is the seventh most common cancer in the world [1], and the second most common cancer in India [2]. Radiation therapy is the main curative treatment in advanced stages [3]. Brachytherapy is a crucial component of radiation therapy for cervical cancer to provide high doses to the tumor while minimizing doses to critical structures [4]. The most often used technique is intra-cavitary brachy-therapy (ICBT), either alone or in combination with interstitial brachytherapy (ISBT). Tandem ovoid (TO)/modified Fletcher suit and tandem ring (TR) applicators are the frequently utilized applicators to provide high-dose-rate (HDR) intra-cavitary brachytherapy [5]. Institutional history in brachytherapy practices, applicator availability, physician expertise, and personal preference, also influence the choice of applicator.
Ring applicators hold an established advantage in terms of maintaining a fixed and reproducible geometry, depicting it a preferred option. Moreover, its flexibility in positioning the radiation source along a 360-degree arc proves advantageous in cases with an antero-posterior spread in the vaginal fornices or cervix. Tandem ovoid finds its niche in patients with oval-shaped or fibrotic upper vaginas, asymmetrical fornix extensions, or narrow introitus but broad vaginal cuffs. Notably, TO is recognized for its ability to deliver greater depth doses compared with TR when applying the same surface dose. While clinical outcomes remain unrelated to applicator choice thus far, understanding these differences aids in optimizing treatment plans and tailoring them to individual patient’s needs.
The choice of applicator depends on patient’s anatomy, residual disease, and unique circumstances, including restricted vaginal canal or complex geometries [6]. A retroverted uterus, which is seen in approximately one in five women [7], is one of the circumstances where the standard TO and TR applicators may cause problems during insertions. Due to its anatomical proximity, the dose received by the rectum tends to be higher; in addition, the applicators are designed for an anteverted uterus, and improper placements, perforations, or bleeding are common to occur [8]. In most institutions, the choice of applicator depends on the preferences of treating doctor, and no strict protocols exist.
In this study, we aimed to evaluate the differences in dosimetry and acute adverse events between the modified Fletcher suit (TO) and ring (TR) brachytherapy applicators in computed tomography (CT)-based intra-cavitary brachytherapy of carcinoma cervix in retroverted uterus.
Material and methods
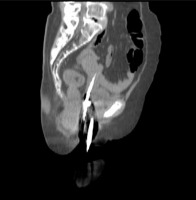
Three hundred seventy-four consecutive intra-cavitary applications (ICAs) performed between November 2021 and August 2023 were investigated retrospectively to identify patients with a retroverted uterus. Only cases where anteversion of the uterus was not possible during application were included (Figure 1). Cases with the modified Fletcher suit applicator were included in group A, and cases with the ring applicator were included in group B. In all applications, the largest possible diameter that could be inserted was applied (20 mm, 25 mm, or 30 mm ovoids for TO, and 20 mm, 40 mm rings with 45° tandem for TR applicator). CT simulation was done on a GE Discovery CT 590 RT scanner, with 2.5 mm thickness slices. Simulation scans and plans were evaluated using Oncentra® Brachy (Elekta). All cases were planned with prescription dose given to point A. Dose calculation was based on TG-43 dosimetric protocol [9]. Prescription doses, D2cc of the bladder and rectum and their mean and median doses, and adverse events, such as severe pain, bleeding, and perforation, were recorded with Elekta Oncentra Brachy™ treatment planning system. Manual optimization of the doses to meet IBS-GEC ESTRO constraints for organs at risk was documented [10]. Pain was described with Wong-Baker faces pain rating scale [11], and the need for additional intravenous analgesics (paracetamol, tramadol), apart from the ones used during anesthesia was documented. Bleeding was categorized as eventful/substantial when blood stained the pack and was noted to be oozing outside the vaginal cavity. Perforation was noted on the simulation CT scan as the complete presence of a part of the central tandem outside the anterior or lateral walls of the uterus [12]. Treatment was delivered using iridium-192 (192Ir) source with activity of 10 Curie (Nucletron, Elekta AB, Stockholm, Sweden).
Statistical analysis
Statistical analysis was completed with JASP (version 0.17.3) and verified using SciPy. Descriptive statistics, with mean and standard deviation were calculated. All data were checked for normal distribution using Kolmogorov-Smirnov goodness-of-fit test. Statistical analysis was done using unpaired student t-test to compare dosimetric differences between the modified Fletcher suit and ring applicators. Differences in symptoms were calculated with z-test for proportions. Significance was assessed at p < 0.05.
Results
Seventy-five applications were eligible for the study among 340 ICAs. The median age of the population was 60 years (range, 33-76 years). In 47 cases, the modified Fletcher suit applicator (group A) was used, and in 28 cases (group B), the ring applicator was applied. Results of the Kolmogorov-Smirnov goodness-of-fit test indicated that there was a non-significant difference in the normal distribution (D (150) = 0.042, p = 0.748). Twenty-nine cases were stage IIB, 8 were stage IIIA, 20 were stage IIIB, 7 cases were stage IIIC, and 5 cases were stage IVA. The dose prescribed to the point A was either 7 Gy × 3 fractions (72 patients) or 9 Gy × 2 fractions (3 patients). Based on the bladder and rectum doses in acceptable applications, the prescription doses were modified, or graphical optimization was done to meet the critical structure constraints. The plans made were approved after ensuring that the point A dose was between 97% and 102%. This was achieved in all the applications (Figure 1).
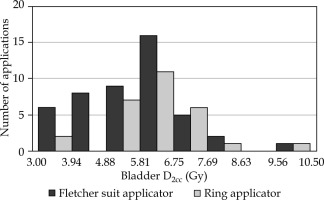
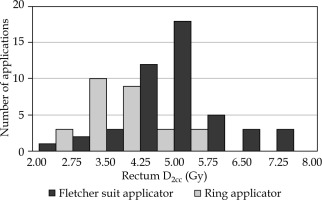
Twenty-five cases in the group A (53.2%) and 20 cases (71.4%) in the group B required optimization, either with dose modification or with graphical optimization. The difference was statistically insignificant (z = –1.5594, p = 0.11876). Table 1 shows the mean and median prescription dose to the point A, bladder, and rectum D2cc.
Table 1
Mean and median prescription dose to point A, bladder, and rectum D2cc
The difference in the bladder D2cc was not statistically significant (p = 0.11, Figure 2). However, there was a statistically significant difference in the rectal D2cc between group A and group B (p < 0.00001, Figure 3). This significant difference was attributed to the presence of rectal separator in the ring applicator.
Eighteen patients in both the groups (38.3% group A and 64.2% group B) complained of pain with given score between 6 and 8 according to the Wong-Baker scale, and required the addition of intravenous paracetamol and/or tramadol after the application done under anesthesia. The z-value was –2.1789, with p = 0.029. Additionally, three cases in the group A and five cases in the group B underwent uterine perforations, and were managed with prophylactic antibiotics, tranexamic acid, and adequate hydration.
Discussion
The applicator geometry plays a key role in brachytherapy, and it has been compared in various studies [13-16]. Anatomy and residual disease designate the choice of the applicator in using the geometry to achieve a good dose distribution. The ring applicator results in significantly elevated surface doses for tissues in close proximity to the source location, particularly the vaginal fornix, when compared with the TO application. Unlike TO applicators, the ring applicator lacks the ability to fine-tune the spacing between its various components. The vaginal ovoid plays a crucial role in shielding the vaginal fornix from receiving a high surface dose [5]. In our study, only the rectal doses were higher when ovoids were used, showing statistical significance. Our results for lower rectal doses with TR matched the outcomes of EMBRACE I study [13]. The increase in pain in the group B patients was found primarily due to the rigid structure of the ring and fixed dimensions, in which it was available as well as the rectal separator. Most women in our studied population tended to have short and stenosed vaginal cavities, where the stretch caused by the applicator components and packing on the vaginal surface were more likely to occur with the ring applicator.
In gynecologic malignancies, patients with a retroverted uterus present a dilemma for brachytherapy because of challenges of procedure and the risk of uterine perforation. Rectal and bladder mean and maximal point doses in ICRU No. 38 vary according to the position of the uterus, with the rectum receiving noticeably greater doses in cases with retroverted uterus [15, 17]. Image-guided brachytherapy can be upgraded to personalized brachytherapy by taking into account the patient’s anatomy, unique applicator geometry, and treatment planning. All these minimize the dose to the organs at risk even more, while greatly improving dose distribution in the target volume. In situations where retroversion can be corrected, the organs are anteverted during uterine sounding, and where it cannot be corrected, it is possible to create satisfactory treatment plans and deliver based on the GEC-ESTRO and Indian Brachytherapy Society (IBS) guidelines. Ultrasound or CT images before applicator’s insertion can help reduce the number of imperfect applications and associated perforations [18]. Therefore, we started performing CT scans before the applications, which provide prior information on the status of the uterus and reduce the imperfect applications and perforations to the minimum. In addition, pre-planning with the available imaging helps to plan the treatment process better [19]. This communication uses recommendations of CT imaging prior to intra-cavitary applications.
The use of ultrasound-guided uterine anteversion for brachytherapy applicator placement is feasible, resulting in acceptable outcome and complication rates, otherwise difficult to manage and at high-risk for uterine perforation. Ultrasound (US) guidance for cervix brachytherapy has been successfully implemented with staff and equipment from radiation oncology. This has led to an improved applicator selection and placement, decreased procedure time, and reduced the number of out-of-department consultations [20]. These changes eliminated repeat insertions due to unfavorable applicator placement (as revealed on post-operative CT); thus, improving department’s efficiency and quality of patient care. The IBS guidelines provide a comprehensive management of carcinoma cervix with emphasis on HDR brachytherapy. The inclusion of applicator selection criteria, especially for retroverted uteri, is a step towards delivering treatment with minimal adverse effects.
We acknowledge the limited parameters studied and retrospective nature of the study. Other parameters, such as D1cc, V85 Gy EQD210, and HR-CTV D90% (EQD210) could provide a better understanding and help in selecting the right applicator for a retroverted uterus. A long-term study is required to assess late toxicities and recurrence rates. In addition, testing the feasibility of various applicators in retroverted uteri using magnetic resonance imaging (MRI)-guided volume-based planning is also a future avenue of research [18].
Conclusions
The tandem ring applicator provides better coverage, with a lesser dose delivered to the rectum as compared with the tandem ovoid applicator, but at the cost of a higher incidence of patient’s pain and discomfort. The two applicators are similar in all the other parameters. The choice of applicator should be made according to patient’s general condition, bladder and rectal doses, and presence of vaginal stenosis, to ensure optimal coverage of the target volumes while minimizing doses to the critical structures and hence, limiting adverse events.