Introduction
Asthma is a chronic respiratory disease, which is characterized by hyperreactivity and airway inflammation [1]. It is estimated to influence about 1-10% of the population worldwide [2]. The pathogenesis of asthma is not fully understood yet, but its risk factors have been identified to be respiratory infections, epigenetic variations, genetics, airborne environmental exposures, atopic conditions and sensitization to inhalant allergens, chemical exposure, microbiome, stress, and metabolites [3]. Severe asthma is heterogeneous and hard to treat, which results in a disproportionate cost to the healthcare systems, and as a result, appropriate management of severe asthma is essential, as most asthma deaths are retrospectively identified as cases of poorly recognized severe asthma [4]. Ongoing studies are searching for better tools of diagnosis and advanced therapy options to decrease the mortality and morbidity related to it, but some patients still suffer from poorly controlled asthma, which may cause life-threatening situations [5]. Therefore, it is of vital importance to investigate the mechanism of asthma to provide efficient treatment for it.
Inhaled corticosteroids (ICS) form the cornerstone of the therapy for asthma, which is of essential importance in achieving asthma control in patients with persistent disease [6]. Fluticasone furoate, budesonide, and fluticasone propionate are ICS approved for asthma pharmacotherapy [7]. ICS can reduce the recruitment and maintenance of inflammatory cells, including dendritic cells, Th2 cells, eosinophils, and mast cells, in the airways of asthmatic patients, which inhibits the production of chemotactic mediators, prevents the expression of adhesion molecules, and inhibits the survival of inflammatory cells in the airway [8-10]. However, when ICS single drug treatment cannot effectively control asthma, other drugs can be used in combination with ICS [11]. Theophylline is one of the most widely applied drugs for the therapy of asthma and in any case, the anti-inflammatory effects and function to reverse corticosteroid resistance of theophylline deserve consideration [12]. Theophylline relaxes smooth muscle located in bronchial airways and pulmonary vessels and also reduces the airway response to histamine, adenosine, methacholine, and allergens [13]. Although different cellular and clinical phenotypes exist in asthma, most studies focus on CD4+ T cells in the context of chronic airway inflammation, which produce a variety of cytokines that may contribute to the underlying inflammation in asthma [14]. While the pathogenic effect of T-helper lymphocytes in asthma progression and persistence is well established, the function of other T cell subsets is uncertain [15, 16]. CD4+ T cell subsets, such as Th1, Th2, and Th17, have shown different contributions to the initiation and persistence of specific asthma phenotypes [17-19]. CD8+ T cells from the peripheral blood have the ability similar to that of CD4+ T cells to produce type 1 and type 2 cytokines, but the role of CD8+ T cells in severe eosinophilic asthma pathobiology is controversial [20, 21]. Theophylline decreases the function of inflammatory reaction and immune cells both in animals with airway inflammation and in humans with asthma [22-25]. Theophylline decreases CD4+CD25+ T, CD4+HLA-DR+ T, CD8+CD25+ T, and CD8+HLA-DR+ T levels in the sputum of asthma patients [26]. However, foreign and domestic studies concentrating on the changes of CD3+CD8+ T cells in peripheral blood of asthma patients in theophylline combined with the ICS treatment process have been comparatively scarce [14]. This study compared the clinical significance of ICS combined with theophylline and ICS alone in the treatment of moderate and severe asthma, so as to provide some reference values for the treatment of asthma.
Material and methods
Ethics statement
The study was authorized by the academic ethics committee of Houjie Hospital Affiliated to Guangdong Medical University. All procedures were strictly implemented according to the Declaration of Helsinki. All subjects involved were fully informed of the objective of the study and signed the informed consent before sampling.
Study subjects
A total of 202 patients with non-allergic moderate to severe asthma treated in Houjie Hospital Affiliated to Guangdong Medical University between May 2021 and May 2022 were included in this study. All patients met the latest GINA standards (https://ginasthma.org/) and did not meet the criteria for allergic asthma [the criteria for allergic asthma were as follows: serum total IgE ≥ 30 IU/ml and ≥ 1 positive permanent aeroallergen-specific IgE value (≥ 0.35 kU/l) at baseline] (https://www.accessdata.fda.gov/drugsatfda_docs/label/2003/omalgen062003LB.pdf). The following perennial allergens were included: pollen, dust mites, house dust mites, Alternaria, Cladosporium, cat and dog dander, Blattella germanica, Blattella orientalis, Aspergillus fumigatus. In addition, 88 healthy people (control group) who underwent physical examination in Houjie Hospital Affiliated to Guangdong Medical University during the same period were selected as the control group. The age range of patients was 18-70 years. All patients had the symptoms (such as asthma, cough, shortness of breath, chest tightness, or pain) 3 days a week during the screening period, and could correctly use the peak flow meter and medication. The pulmonary function test was performed immediately after patients’ enrollment, and 5 ml of fasting venous blood was collected in the morning of the next day after enrollment. Basic information such as gender, age, body mass index (BMI), smoking history, and basic level of lung function was recorded at the first visit. The experimental group (ICS + THEO) received 250 µg fluticasone aerosol (BID, 125 µg/inhalation) combined with 0.2 g theophylline (BID, 0.1 g/tablet). The treatment control group (ICS) received 250 µg fluticasone aerosol (BID, 125 µg/inhalation) combined with 0.2 g BID placebo. Patients were allowed to use salbutamol aerosol as temporary relief throughout the study period.
The exclusion criteria were as follows: 1) with severe heart or lung disease; 2) respiratory tract infection within 8 weeks; 3) taking systemic steroids or anticholinergic drugs, long-acting β agonists, or leukotriene receptor antagonists within 6 weeks; 4) allergic to drugs; 5) pregnant or lactating women; 6) abnormal urine, blood, and biochemical tests; 7) participating in the trials of other drugs; 8) with a history of life-threatening asthma and other important lung diseases within 6 months after screening.
Fractional exhaled nitric oxide
Fractional exhaled nitric oxide (FeNO) of all subjects was evaluated using the FeNO detector (NIOXMINO, Aerocrine, Sweden) according to the recommendations of the European Respiratory Society (ERS) and the American Thoracic Society (ATS) [27]. FeNO was measured before spirometry.
Pulmonary function test
Forced expiratory volume (FEV1), forced vital capacity (FVC), and peak expiratory flow (PEF) of all subjects were measured in 1 s using a spirometer (Spirolab, Italy). The best value of the 3 maneuvers was selected as the absolute value of the predicted value.
Symptom control and quality of life assessment
The asthma symptom control of patients was assessed using the asthma control test (ACT), a 5-item questionnaire on the impact of asthma on family and work activities, shortness of breath, symptoms, first aid drug use, and overall asthma control. The score range was 5-25 (a high score indicated that the patient’s asthma symptoms were well controlled), with 20-25 indicating that the asthma was well controlled, 16-19 indicating that the asthma was not well controlled, and 5-15 indicating that the artificial asthma control was very poor [28].
The quality of life of patients was evaluated using the standardized version of the Asthma Quality of Life Questionnaire (AQLQ), which consisted of 4 domains (symptoms, activity restriction, emotional function, and environmental stimulation), with a total of 32 items. The total score was the average of these 32 items, ranging from 1 (severe injury) to 7 (no injury) [29].
Blood eosinophil count
Eosinophils in peripheral blood samples were counted and the percentage was calculated using a multifunctional automatic blood analyzer (Sysmex, Kobe, Japan).
ELISA
5 ml of fasting venous blood was collected from the subject, of which 2 ml was collected in a common test tube and centrifuged at 3000 g for 10 min, and the serum was collected and placed into Eppendorf tubes with a volume of 0.5 ml, labeled and stored at –80°C. IL-4 (# BMS225-2, sensitivity: 1.3 pg/ml, determination range: 7.8-500 pg/ml), IL-6 (# BMS213-2TEN, sensitivity: 0.92 pg/ml, determination range: 1.56-100 pg/ml) and IL-12 (# KAC1568, sensitivity: 0.2 pg/ml, determination range: 1.56-100 pg/ml) levels were determined by ELISA. The sample processing, determination and content calculation were strictly performed according to the instructions of the kit, which was purchased from Thermo Fisher Scientific (Waltham, MA, USA).
Preparation and storage of PBMCs
3 ml peripheral blood samples were collected in tubes containing ethylenediamine tetraacetic acid (EDTA) anticoagulants (BD vacutainer EDTA tubes, BD Biosciences, San Jose, CA, USA) and treated within 8 h [30]. Briefly, blood was added to the same volume of Ficoll Histopaque-1077 (Sigma-Aldrich, Louis, MO, USA) in a 50 ml conical tube, and centrifuged at 400 × g in a cradle rotor without brakes for 30-40 min. The PBMC layer was transferred to a new 50 ml conical tube (Corning, Sigma-Aldrich), added to 15 ml of RPMI 1640 medium (Thermo Fisher), and centrifuged at 1000 × g for 10 min. To remove platelets, the cell particles were resuspended in 50 ml of medium and centrifuged at 20°C at 200 × g for 10-15 min, and the supernatant was completely removed. Live cells were counted in a Burker chamber. After storage at –20°C for 1 h, the aliquot of 3 × 106 cells was stored in liquid nitrogen in 2 ml of cryopreserved solution containing RPMI 1640 medium (Gibco-Thermo Fisher Scientific) 10% DMSO and 10% of FBS overnight until flow cytometry. Flow cytometry was carried out after thawing under the same conditions.
Detection of lymphocytes by flow cytometry
Blood samples were processed by flow cytometry using a monoclonal antibody kit (BD Multitest 6-color TBNK, San Jose, CA, USA), including FITC-labeled CD3+ T, PE-Cy7-labeled CD3+CD4+ T and APC-Cy7-labeled CD3+CD8+ T. Multi-test 6-color TBNK was employed to identify lymphocytes, which were distinguished according to forward (FSC) and lateral (SSC) scattering. Subsequently, the dead cells were removed using the 7-AAD labeling method, and the adhesive body was eliminated using FSC-A and FSC-H. Furthermore, SSC and CD45 were used for additional gating to distinguish lymphocytes and cell fragments. Subsequently, specific panels were assessed to identify T lymphocytes. T lymphocyte subsets were gated to distinguish CD3+CD4+ T (T-helper) and CD3+CD8+ T (T-cytotoxic). The gating strategy is shown in Supplementary Figure 1. Events were collected using diva software (BD Biosciences) and a FACS CantoII (BD Biosciences) cell analyzer, and data were analyzed using Kaluza Analysis 2.1 software (Beckman and Coulter, Fullerton, CA, USA).
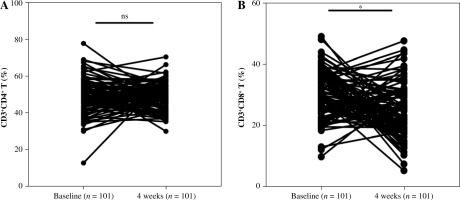
Fig. 1
Effect of theophylline combined with ICS on T lymphocyte subsets in peripheral blood of patients with moderate and severe asthma. A) Percentage of CD4+ T cells in peripheral blood was assessed by flow cytometry; B) Percentage of peripheral blood CD8+ T cells. Baseline: newly enrolled patients in the ICS + THEO group without any treatment, 4 weeks: patients in the ICS + THEO group who received 4 weeks of treatment. Independent sample t test was adopted for comparison between 2 groups. ***p < 0.001
Statistical analysis
SPSS 24.0 (IBM Corp. Armonk, NY, USA) and GraphPad Prism 8.01 (GraphPad Software Inc., San Diego, CA, USA) were applied for statistical analysis and mapping. For normally distributed continuous variables, data were expressed as mean ± standard deviation (SD). For non-normally distributed variables, data were expressed as median and interquartile range. For categorical variables, data were expressed as numbers (percentages). The Kolmogorov-Smirnov test was adopted to evaluate normal distribution of continuous variables. The chi-square (χ2) test was employed to analyze the difference of categorical variables. When continuous variables were normally distributed, the independent sample t test was applied for analysis between two groups; the Mann-Whitney U test was applied for the comparisons between two groups with non-normal distribution. When the continuous variables were normally distributed, the differences between groups were tested by one-way analysis of variance (ANOVA), and the differences between groups of non-normal distribution were tested by the Kruskal-Wallis test. Pearson correlation was used to analyze the correlation between CD3+CD8+ T cells and clinical indexes. The p value was obtained by a bilateral test. P < 0.05 indicated statistical significance.
Results
Clinical baseline data
A total of 202 patients with moderate to severe asthma who met our criteria and 88 healthy subjects (control) participated in this study. Among the patients, 101 were treated with ICS combined with theophylline (ICS + THEO group), and the other 101 were treated with ICS alone (ICS group). The clinical baseline data of all subjects are shown in Table 1, and there were no significant differences between the healthy control group and the patients in terms of sex, age, BMI, and smoking or not, but there were significant differences between the healthy control group and the patients in terms of FeNO, FVC, FEV1, PEF, eosinophils, and serum IL-4, IL-6, IL-12 levels (p < 0.05).
Table 1
Clinical baseline data of patients with moderate and severe asthma
[i] BMI – body mass index, FeNO – fractional exhaled nitric oxide, FVC – forced vital capacity, FEV1 – forced expiratory volume in 1 second, PEF – peak expiratory flow, ACT – asthma control test, AQLQ – Asthma Quality of Life Questionnaire. For normally distributed continuous variables, the data were described by mean ± standard deviation (SD); for non-normally distributed variables, data were described by median and interquartile range (IQR); for categorical variables, data were described as numbers (percentages). The χ2 test was used to analyze the differences of categorical variable among the groups. For continuous variables with normal distribution, one-way ANOVA was used to detect the differences between groups. For continuous variables with non-normal distribution, the Mann-Whitney U or Kruskal-Wallis test was used to detect the differences between groups. Note: a indicated that compared with the control group, p < 0.05.
Theophylline improved the effect of ICS on asthma
After 4 weeks of treatment, the lung function and life quality scores of patients were assessed again. Compared with the ICS group, the FeNO value, the number of blood eosinophils, and the levels of IL-4 and IL-6 in the ICS + THEO group were decreased (Table 2, all p < 0.05), and FVC, FEV1, PEF, and IL-12 levels were increased (Table 2, all p < 0.05).
Table 2
Theophylline enhanced the therapeutic effect of ICS on asthma
[i] FeNO – fractional exhaled nitric oxide, FVC – forced vital capacity, FEV1 – forced expiratory volume in 1 second, PEF – peak expiratory flow, ACT – asthma control test, AQLQ – Asthma Quality of Life Questionnaire. For continuous variables with normal distribution, the data are expressed as mean ± standard deviation (SD). For non-normal distribution variables, data were expressed as the median and interquartile range (IQR); for classification variables, data were expressed as quantity (percentage). For continuous variables with normal distribution, the independent sample t-test was used to detect the differences between two groups, and the Mann-Whitney test was used to detect the differences between groups for continuous variables with non-normal distribution.
In addition, the scores of asthma control test and Asthma Quality of Life Questionnaire in the ICS + THEO group were significantly higher than those in the ICS group (Table 2, all p < 0.05).
Theophylline combined with ICS reduced the percentage of CD8+ T cells in peripheral blood of patients with moderate and severe asthma
The percentage of peripheral blood T lymphocyte subsets was assessed by flow cytometry. There was no significant difference in the absolute quantity and percentage of CD3+CD4+ T cells (Fig. 1A, Table 3, p > 0.05), while the percentage of CD3+ T cells and CD8+ T cells was reduced after ICS combined with theophylline treatment (Fig. 1B, Table 3, all p < 0.05). The results suggested that theophylline combined with ICS reduced the absolute number and percentage of CD3+ T cells and CD3+CD8+ T cells in peripheral blood of patients.
Table 3
Changes of T-lymphocyte subsets in peripheral blood of patients with moderate and severe asthma after theophylline combined with ICS
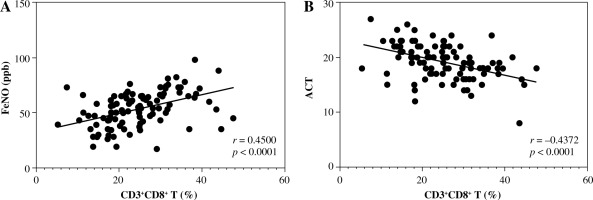
Peripheral blood CD8+ T cells were correlated with lung function and asthma symptom control in patients with moderate and severe asthma after drug combination therapy
To further explore the relationship between peripheral blood CD3+CD8+ T cells, lung function, and quality of life in patients treated with combination therapy, Pearson correlation was employed to analyze it. CD3+CD8+ T cells in peripheral blood were positively correlated with FeNO (Fig. 2A, r = 0.4500, p < 0.0001) and negatively correlated with ACT (Fig. 2B, r = –0.4372, p < 0.0001). The results suggested that CD8+ T cells in peripheral blood of patients with moderate and severe asthma after receiving drug combination therapy were positively correlated with lung function and negatively correlated with asthma control.
Fig. 2
Correlation analysis of peripheral blood CD8+ T cells with lung function and asthma symptom control parameters in patients with moderate and severe asthma after drug combination therapy. Pearson correlation analysis was employed to assess A) the correlation between peripheral blood CD3+CD8+ T cells and FeNO; B) the correlation between CD3+CD8+ T cells and ACT. Here were patients in the ICS + THEO group after 4 weeks of treatment (n = 101)
Discussion
Asthma is a frequent chronic respiratory disease all over the world, with an increase in prevalence in the last decade [5]. Evidence has revealed that ICS is the mainstay of asthma pharmacotherapy [7]. Theophylline has been applied in the therapy of asthma, which has remained the most commonly prescribed anti-asthma drug for several decades all over the world [31]. Low-dose theophylline can increase the accumulation of histone deacetylase in epithelial cells and macrophages [32, 33] and has a synergistic anti-inflammatory effect combined with ICS [34]. However, theophylline alone improves the asthma control questionnaire score, but not lung function [34]. This study revealed that theophylline improved the therapeutic effects of ICS on asthma and reduced inflammation level and the content of CD3+ T and CD3+CD8+ T cells in peripheral blood of patients with moderate and severe asthma.
Inhaled corticosteroid has improved the lives of people with asthma, as it can reduce or abolish the symptoms, and reduce the risk of exacerbations [35]. Theophylline has immunomodulatory and anti-inflammatory functions and can reduce eosinophilic inflammation, showing great potential for treating chronic asthma [36]. Fractional concentration of FeNO in exhaled air is a good biomarker for type 2 airway inflammation [37]. Elevated blood eosinophilia in conjunction with FeNO level is a treatable trait of type 2 inflammation of asthma, and FeNO level is related to bronchial eosinophilic inflammation and airway hyper-responsiveness [38]. During asthma exacerbation, facilitated airway resistance is accompanied by reduced spirometry values (FEV1, FVC, and PEF) [39]. Considerable evidence has shown that the inflammation of the airway is a main factor in asthma pathogenesis [40]. The quality of life in asthma patients is measured using the AQLQ tool [41]. Asthma is “controlled” when lung function is improved, while failure to achieve control is associated with a decrease in lung function and deterioration in quality of life [42]. Our results showed that after 4 weeks of treatment, the FeNO value, the blood eosinophil count, and IL-4 and IL-6 levels were repressed, PEF, FEV1, FVC and IL-12 level were augmented, and the AQLQ score was increased in patients treated with theophylline combined with ICS, indicating a better recovery in lung function, a more obvious asthma symptom regression, and a better improvement in quality of life. Consistently, obvious repression in the mean levels of FeNO is found in mild, moderate, and severe cases of asthma following ICS treatment [43]. The improvement of spirometric parameters such as FEV1, FVC and PEF values is observed in asthma patients after ICS treatment [44], after theophylline treatment [45], or treatment with theophylline combined with ICS [46]. Similarly, low-dose theophylline addition may be equal to doubling ICS dose in the treatment of asthma not adequately controlled by a low dose of ICS [47]. Low-dose theophylline further improved asthma control in patients already treated with ICS [48]. This study showed that theophylline improved the effects of ICS on asthma.
Our study initially found that the levels of IL-4 and IL-6 in peripheral blood of asthmatic patients were increased, while the level of IL-12 was decreased. CD4 T cells also play roles in autoimmunity, allergic responses, and asthma as well as in tumor immunity. During the activation of TCR in a particular cytokine milieu, naive CD4 T cells can differentiate into one of the several Th cell lineages, such as Th2, Th1, iTreg, and Th17, as defined by their pattern of cytokine production and function [49]. It is well known that Th1/Th2 disproportionation is the main cause of asthma [50]. IL-4 is a powerful inflammatory response activator, considered as the central Th2 cytokine of the immune system, and plays an important role in fibrosis during Th2 inflammation [51]. In patients with asthma, Th2 is overactive, and there are increased levels of IL-4 and IgE, which stimulate the proliferation and activation of eosinophils and secretion of various inflammatory mediators, leading to chronic bronchial inflammation and asthma [52]. A previous study showed that IL-4 is significantly overexpressed in the acute and plateau phases of asthma, suggesting that immune dysfunction is involved in the occurrence and development of asthma [53]. IL-4-promoted an abnormal increase of IgE, which has been proved to be one of the pathogeneses of asthma, suggesting that IL-4 may indirectly induce asthma [54]. IL-6 is a multifunctional cytokine produced by active macrophages and monocytes. IL-6 may increase IL-4 during Th2 differentiation, induce inflammation, and may be a potential promoter of lung diseases such as asthma [55]. The overexpression of IL-6 is related to the obstruction of fixed air flow, and IL-6 overexpression is also found in the bronchial epithelial cells of adults and children with asthma [56]. In addition, activated monocyte-macrophages, dendritic cells, and other antigen-presenting cells can produce bioactive IL-12. IL-12 is the key cytokine for Th0 to Th1 differentiation. The increase of IL-10 in asthma patients can promote the Th2 response by reducing IL-12 [57]. IL-12 is a potential therapeutic method for asthma, and IL-12 deficiency is one of the basic underlying mechanisms of the specific response [58].
CD3+CD4+ T cells produce a variety of cytokines, which may contribute to the underlying inflammation in asthma [14]. CD3+CD8+ T cells are increasingly proposed to have a vital function in the pathogenesis of asthma, because they are abundant and comparatively insensitive to corticosteroids [59]. Our results revealed that there was no significant difference in CD3+CD4+ T cell absolute quantity and percentage, while CD3+ T and CD8+ T cell percentage was suppressed after ICS combined with theophylline treatment. Consistently, a significant fall in peripheral blood monocytes activated CD8+ T cells in patients with plasma theophylline > 5 mg/l [60]. ICS treatment prevents the response of CD8+ T cells in a mouse model of allergic asthma [61]. In brief, theophylline combined with ICS treatment suppressed CD8+ T cell absolute quantity and percentage in peripheral blood of asthma patients. Furthermore, we discovered that CD3+ T and CD3+CD8+ T cells in peripheral blood were positively correlated with FeNO and negatively correlated with ACT.
In summary, we analyzed the efficacy and peripheral blood T lymphocyte subsets of 101 patients with moderate to severe asthma who received theophylline combined with ICS therapy. As expected, lung function and quality of life were improved after 4 weeks of treatment. At present, there is still little research on CD3+CD8+ T cells in asthma patients. IL-4 acts as an important pro-inflammatory cytokine in the immune regulation mediated by activated T helper cells (Th) and promotes the transformation of immunoglobulin E isoforms of B cells [62]. IL-6 is a small glycoprotein (21 kDa) that acts on epithelial cells and immune cells. It is produced by cells from the innate immune system, including macrophages, dendritic cells, mast cells, and neutrophils. Previous studies have shown that IL-6 can cause asthma and other lung diseases by increasing airway mucus hypersecretion [63, 64]. IL-12 is a heterodimer composed of α and β subunits (called p35 and p40 respectively), which is characterized by producing interferon γ, which is also an important cytokine in anti-tumor immunity, and promotes anti-tumor immunity by activating natural killer cells and Th1 T cells [65]. This study analyzed the correlation between CD3+CD8+ T cells and the lung function of patients after treatment, and concluded that the percentage of CD3+CD8+ T cells was related to lung function and asthma control. However, there are still limitations of this study. In view of the significant difference in the number of CD3+CD4+ T cells, we believe that the reasons for this are as follows: 1) The local inflammation of the respiratory tract detected by peripheral blood is slightly insufficient [26]. 2) The number of patients included in this study may be too small. Furthermore, we did not conduct a follow-up on the disease status and quality of life of the patients, and the long-term status of asthma patients was neglected. In the future, we will simultaneously study the changes of lymphocytes in peripheral blood and sputum, and expand the clinical sample size to more comprehensively explore the effect of theophylline combined with ICS on lymphocytes in asthma patients. In addition, we will further follow up on the changes in disease grade, lung function, and quality of life of asthma patients after treatment.