Introduction
Simultaneously cerebral and coronary angiography (SCCAG) was first reported in 1991 [1], and many studies are currently focusing on this topic [2, 3]. Compared with transfemoral artery access (TFA) for angiography, transradial access (TRA) has fewer complications, is easier to compress to stop bleeding, reduces bed rest time, and is more comfortable for patients [4]. Therefore, TRA has been recommended by relevant guidelines [5–7].
With the continuous development and change of the selection of puncture sites, a large number of studies have emerged to compare the advantages and disadvantages of different approaches. The transfemoral approach is easy to operate and has a high success rate, but it is prone to complications such as vagal reflex and pseudoaneurysm, the lower limb on the puncture side needs to be immobilized after the operation, the patient will stay in bed for a long time, and they may also experience constipation and inconvenient urination [8]. Elderly patients may also have lower extremity venous thrombosis due to prolonged bed rest, which is unfavourable for their prognosis [9]. After the radial artery intervention, the arterial sheath can be removed immediately without breaking, the body position is not high, and the difficulty of haemostasis is relatively low, which can effectively shorten the bed rest time, relieve the pain of the patient, and reduce the occurrence of local complications such as pseudoaneurysm [10]. So far, the effect of different puncture points on perioperative complications and length of stay in hospital (LOS) in SCCAG patients has rarely been reported.
Aim
The purpose of this study was to compare the efficacy and safety of transradial and transfemoral approaches in combined cardio-cerebral angiography.
Material and methods
Patient selection and study design
A total of 120 patients who received combined heart-brain angiography in our hospital were selected and divided into a TRA group and a TFA group according to the random number table method. Both groups received combined heart-brain angiography. The TRA group (n = 60) was treated via the radial artery, and the TFA group (n = 60) was treated via the femoral artery. Patients signed informed consent forms for coronary angiography or stent, cerebral angiography, and stent. The study was approved by the Medical Ethics Committee of Peking University International Hospital.
Inclusion and exclusion criteria
Inclusion criteria: patients with intracranial and extracranial vascular stenosis detected by non-invasive imaging methods and patients with moderate or greater coronary stenosis, who needed to undergo both cerebral angiography and coronary angiography at the same time for diagnosis or treatment. The puncture path was selected according to the following criteria: 1. Inclusion criteria for radial artery access: the preoperative modified Allen test was positive and the diameter of the radial artery was > 2 mm by ultrasound evaluation. 2. Inclusion criteria of femoral artery route: patients with stenosis or obstructive lesions in peripheral arteries, Raynaud’s phenomenon, hand trauma and/or surgery history, known arm anatomical variation, radial artery as a blood vessel for coronary artery bypass grafting or dialysis treatment. Exclusion criteria were as follows: patients who needed second-stage treatment after combined heart-brain angiography; the second-stage treatment includes carotid artery, vertebral artery, subclavian artery stent implantation, coronary artery stent implantation, coronary artery stent surgery, and carotid endarterectomy; acute myocardial infarction, acute cerebral infarction, and other patients requiring emergency surgery; patients in cardiogenic shock; patients with severe hepatic and renal insufficiency; and patients with coagulation disorders.
Operation
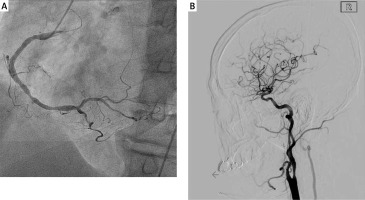
According to the patient’s department, if unstable angina is the first symptom, coronary angiography should be performed first. If ischaemic stroke is the first symptom, cerebral angiography should be performed first; after local anaesthesia at the puncture point, a radial artery puncture needle should be used to puncture the wall. Puncture the femoral artery with “non-transmural method”. After successful puncture, the loach guide wire was used to guide the corresponding catheter for operation. For whole cerebral angiography via the radial artery route, a 260-cm loach guidewire, pigtail catheter, and SIM-2 catheter were selected for vessel selection. After the long loach guide wire guided the pigtail catheter into the ascending aortic arch, ascending aortic angiography was performed to clarify the blood vessels on the aortic arch. Then, with the help of the pigtail catheter, a 260-cm loach guide wire was introduced into the distal end of the descending aorta, and the loach guide wire was retained. After withdrawing the pigtail catheter, the SIM-2 catheter was inserted. Superselective cerebral angiography was performed after the descending aorta was used. Coronary angiography and surgery were performed by the Department of Cardiology, and cerebral angiography was performed by interventional neurologists. Intervention operations were performed by senior attending physicians with intervention qualifications (Photo 1).
Indicators
Surgery-related indicators were as follows: puncture time, operation time, postoperative bed rest time, hospitalization time, and X-ray exposure time. Cardiac function indicators were as follows: left ventricular ejection fraction and complication rate (urinary retention, vagal reflex, vasospasm, haematoma, false aneurysm).
Ethical approval
Patients signed informed consent for coronary angiography or stent, cerebral angiography, and stent. The study was approved by the Medical Ethics Committee of Peking University International Hospital.
Statistical analysis
SPSS 25.0 statistical software was used for analysis. Measurement data were expressed as mean ± standard value, and the t-test and rank-sum test were used, respectively. Categorical variables were described by frequency (rate), and the χ2 test or Fisher’s exact probability method was used. A statistically significant difference was considered to be p < 0.05.
Results
Patients’ general information
There were 120 patients, aged 39–81 years, with an average age of 60.31 ±8.32 years. Among them, 66 (55.0%) were male, 59 (49.2%) were smoking, 53 (44.2%) were drinking, 58 (48.3%) had hypertension, 49 (40.8%) had diabetes, 35 (29.2%) had hyperlipidaemia, and 2 (1.7%) cases had peripheral vascular disease (Table I).
Table I
Baseline clinical characteristics
Surgery-related indicators
There was no statistically significant difference in puncture time and operation time between the 2 groups (p > 0.05); postoperative bed rest time, hospitalization time, and X-ray exposure time in the TRA group were shorter than those in the TFA group, and the difference was statistically significant (p < 0.05) (Table II).
Table II
Surgery-related indicators
Cardiac function indicators
We compared preoperative and postoperative left ventricular ejection fraction in the 2 groups of patients. Before operation, there was no difference in left ventricle ejection fraction (LVEF) between the 2 groups, and 3 days after operation, there was still no significant difference in LVEF between the 2 groups (p > 0.05) (Table III).
Complications
We observed the incidence of postoperative complications in the 2 groups of patients. It can be seen that the overall incidence of complications in the TFA group was higher than that in the TRA group. The incidence of haematoma and pseudoaneurysm in the TFA group was higher, and the difference was statistically significant (p < 0.05), which was the main contribution to the increase in overall complications (Table IV).
Table IV
Incidence of complications
Discussion
Atherosclerosis mainly occurs in the large and medium arteries in the body, especially the cerebral arteries and coronary arteries. They often occur at the same time, and have the common characteristics of thickening, hardening, loss of elasticity, and contraction of the arterial wall. Clinically, when coronary artery stenosis and carotid artery stenosis coexist, the current treatment options mainly include simultaneous treatment and staged treatment. When cerebral arteries are also severely stenotic, whichever procedure is performed first carries high perioperative risks. Therefore, in this case, both lesions should be treated simultaneously. Since the treatment regimens and medication strategies of the 2 diseases are similar, it is relatively easy to achieve combined treatment. From our research results, no matter whether the patients are treated via radial artery or femoral artery, the LVEF of the 2 groups can be effectively improved, and there is no difference between the 2 methods, which shows that the radial artery and femoral artery intervention can both guarantee the therapeutic effect of patients and improve vascular function. But we found that TRA had a shorter operation time, and the patients’ bed rest and hospital stay were shorter.
TRA diagnosis and treatment of the coronary artery is very mature, but the time of neurointerventional diagnosis and treatment is still short. Cerebral angiography by TRA was first reported around 2000 [11, 12]. Cerebral angiography via the femoral artery is a traditional clinical approach with long application experience, and because the internal diameter of the femoral artery is large, it has a high success rate in puncture, and the difficulty of clinical operation is low, so it has been widely used clinically. With the development of clinical application, the problems of this approach are constantly exposed. For example, postoperative immobilization time of patients should be more than 24 h, and postoperative patients are prone to pseudoaneurysm and large haematoma at the puncture site [13]. Obese patients will increase the difficulty of puncture and haemostasis, and patients are more prone to pseudoaneurysm. Furthermore, the transfemoral approach is not indicated for patients with spinal deformities [14]. In recent years, with the continuous improvement of interventional diagnosis and treatment technology, more and more medical centres have begun to use TRA as an optional path for nerve interventional diagnosis and treatment, and they even use TRA as the preferred puncture method [15, 16]. Authors [17] reported a meta-analysis about the relative safety of cerebral angiography procedures conducted via transradial and transfemoral approaches. The study results suggested that both TRA and TFA cerebral angiography strategies can yield similar rates of success when performing cerebral angiography, with TRA being associated with a shorter duration of postoperative recovery and lower complication rates (radial artery bleeding, haematoma, compartment syndrome, radial artery spasm, and radial artery occlusion). However, the study did not include the supra-aortic and branch vessel data. We believe that the therapeutic effect is related to the proficiency of the operation and the severity of the disease. It has been suggested that the risk of complications is higher when treating both cerebral and coronary artery disease than when treating a single lesion. However, the results of this study showed that postoperative complications did not increase, indicating that combined heart-brain angiography has good safety. The RIVAL study is a multicentre randomized double-blind controlled study that compared the complication rates of TRA and TFA in patients undergoing coronary artery diagnosis and treatment. The study showed that TRA-related complications were lower than those of TFA [18]. In our study, the overall complication rate of TFA was 18.3%, with haematoma and pseudoaneurysm as the main causes. The patient with haematoma at the puncture point improved after haemostasis by recompression, bandaging, and bed rest, without special treatment. The complication rate of TRA group was 8.3%, which was significantly better than that of TFA. In 2021, the results of a Chinese study were consistent with ours, showing that the total complications of vascular puncture in SCCAG patients in the TRA group were less than those in the TFA group [2].
The length of stay is an important indicator for evaluating the utilization efficiency of medical centres, and many studies have focused on the influencing factors of LOS [19, 20]. Previous studies have shown that TFA patients need to stay in bed after surgery, while TRA patients have good haemostatic effect and do not need to stay in bed, which will inevitably lead to a significant reduction in LOS, and even meet the requirement of being discharged on the same day [21]. This study also suggested that, in terms of SCCAG patients, LOS was less in the TRA group. This not only helps to increase the comfort of patients, but can also effectively save medical resources under the premise of the current shortage of medical resources, and create a more convenient medical environment for more patients with urgent needs at the same time.
There are some limitations in this study. First, this study is a single-centre study, which only reflects the initial experience of using TRA to perform SCCAG in this centre. Second, the number of data included is small. In the next step, we will continue to include data on the basis of this study for further discussion. In conclusion, according to the data of this study, TRA puncture for SCCAG is clinically feasible, relatively safe, and can reduce the hospitalization time of patients.
Conclusions
For simultaneous heart-brain angiography, interventional therapy via radial artery and femoral artery has good curative effect and can improve cardiac function. However, interventional therapy through the radial artery can shorten the postoperative bed rest time and hospitalization time, and reduce the incidence of complications.