Introduction
Epidural analgesia (EA) has decreased systemic opioid usage as the favoured method for postoperative pain release after elective open abdominal surgery during the past 20 years [1]. Also, EA has better analgesic effectiveness and is related to significantly lower rates of illness and death [2]. Epidural analgesia causes better postoperative ventilation and opioid sparing, and decreased insulin resistance [3], and it is a central constituent of enhanced recovery after surgery (ERAS) because of its origin [4]. Although the risk of procedural problems, e.g. epidural haematoma, is infrequent post-EA, postoperative hypotension is common and might cause augmented intravenous fluid management and stop initial postoperative mobilisation [5]. Recently, interest has been growing in the use of wound catheter (WC) for local anaesthetic infiltration (LAI) as a substitute for EA after open abdominal surgery, and data from randomised controlled trials shows that the postoperative pain scores are similar [6]. Wound catheters avoid the risks related to EA, mainly postoperative hypotension, and have come to be standard practice through open hepatectomy (OH) in some healthcare centres [7]. A randomised controlled trial (RCT) by Hughes et al. indicated that WCs were related to faster recovery after OH compared with epidural analgesia [8]. This discovery was not simulated by the latest study by Bell et al. [9].
This study aimed to appraise the influence of WC LAI compared with EA in OH. Laparoscopy has documented advantages compared to traditional open abdominal surgery, such as decreased pain, fewer wound problems, and shorter hospitalisation periods [10]. The utilisation of minimally invasive surgery (MIS) in liver resection has increased alongside the improvement in safety and the prevalence of surgical excision for both benign and malignant liver tumours [11, 12]. Multiple studies have provided evidence of the efficacy of MIS in liver resection, demonstrating less intraoperative blood loss, decreased incidence of bile leak, and fewer sequelae [13–16]. The available evidence for MIS hepatectomy comes primarily from research with patients who underwent non-anatomic or small liver resections (including 2 or fewer contiguous Chouinard segments). Additionally, most studies on MIS did not involve high-risk resections [17, 18].
Aim
In the field of occupational health, the purpose of this study was to evaluate the impact of wound catheter local anaesthetic infiltration in comparison to epidural analgesia in open hepatectomy.
Material and methods
Study design
The epidemiological declaration [19] was the subject of the present meta-analysis, which encompassed studies that tracked a prearranged study technique [20].
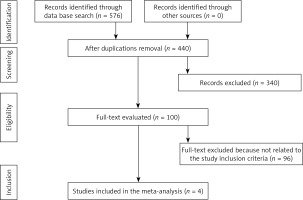
Figure 1 illustrates the whole sequence of the study.
Identification
First we conducted a literature search up to March 2023 using a blend of keywords and similar words for open hepatectomy, wound catheter local anaesthetic infiltration, epidural analgesia, opiate consumption on the second postoperative day, overall complication rate, pain score on the second postoperative day, and functional recovery time, as shown in Table I [21].
Table I
Search strategy for each database
Screening
Data were reduced based on the procedure of previous meta-analysis studies [22]. When there were dissimilar data from one study based on the calculation of the consequence of WC LAI compared with EA in OH, we extracted them independently. The two writers independently assessed the methodologies of the chosen publications to assess the potential bias in each study. The methodological quality was appraised using the “risk of bias instrument” from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.13 [23].
Eligibility
The main focus was the calculation of the outcome of WC LAI compared with EA in OH, and an analysis of the WC LAI compared with EA was extracted to form a summary.
Inclusion criteria
Included studies had to be randomised clinical trials or retrospective studies. In addition, the design of these studies had to be based on a comparative design between different anaesthesia techniques.
Exclusion criteria
Studies were excluded in certain cases: studies written in other languages, studies in the form of letters, communications, and book chapters.
Statistical analysis
The odds ratio (OR) and mean difference (MD) with a 95% confidence interval were calculated in the current meta-analysis using a random- or fixed-effect model with dichotomous and contested methods (CI) [24]. All p-values were calculated using 2-tailed tests. The statistical analysis and graphs were performed/drawn with Reviewer Manager version 5.3. A random-effects model was fitted to the data. Using the constrained maximum-likelihood estimator, the level of heterogeneity (χ2) was calculated. The I2 index was computed, with a range from 0 to 100, conveyed in the form of forest plots. This index was obtained using Reviewer Manager software. The heterogeneity level was shown by percentages ranging from 0% to 100%, indicating low, moderate, and high levels of heterogeneity. Begg’s and Egger’s tests were used to conduct quantitative research on publication bias, and the presence of publication bias was deemed to be present if p > 0.05.
Results
A total of 576 pertinent studies were found, of which 4 studies between 2012 and 2022 met the inclusion criteria and were elaborated in the meta-analysis as shown in Table II [7–9, 25].
Table II
Characteristics of the studies selected for the meta-analysis
| Study | Country | Study design | Total | Wound catheter local anaesthetic infiltration | Epidural analgesia |
|---|---|---|---|---|---|
| Revie, 2012 [7] | UK | RCT | 64 | 33 | 31 |
| Hughes, 2015 [8] | UK | RCT | 93 | 49 | 44 |
| Bell, 2019 [9] | UK | RCT | 83 | 42 | 41 |
| Jackson, 2022 [16] | UK | Retrospective observational study | 110 | 35 | 75 |
| Total | 350 | 159 | 191 |
The designated studies encompassed 350 subjects with OH at the baseline of the studies; 159 of them were managed with WC LAI, and 191 used EA. The size of the studies ranged from 64 to 110 subjects at the start of the study.
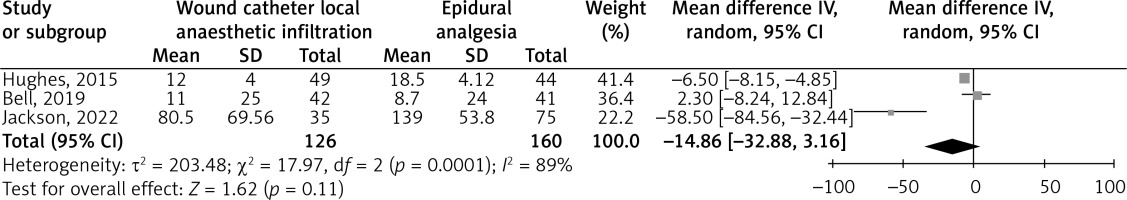
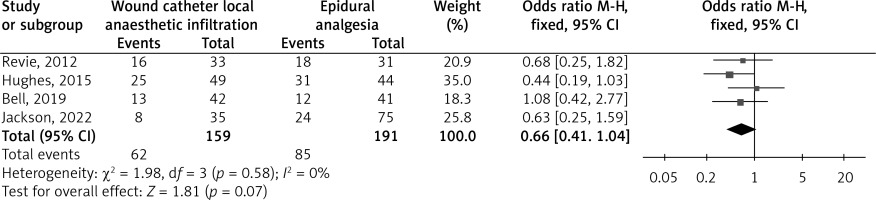
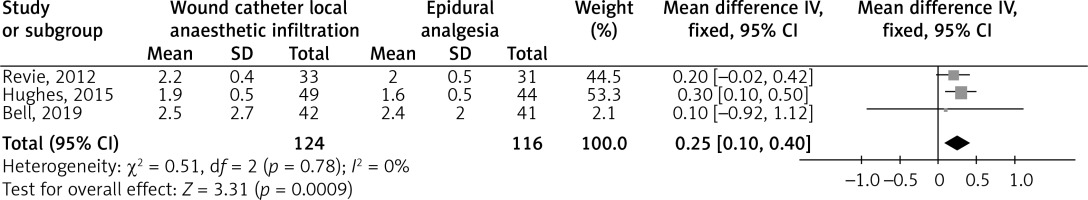
The use of WC LAI resulted in a significantly lower Functional Recovery Time (MD = –0.64; 95% CI: –1.02 to –0.26, p < 0.001) with no heterogeneity (I2 = 0%), and higher pain score on the second postoperative day (MD = 0.25; 95% CI: 0.10–0.40, p < 0.001) with no heterogeneity (I2 = 0%) in subjects with OH compared with EA, as shown in Figures 2 and 3. However, WC LAI did not show any significant difference in opiate consumption on the second postoperative day (MD = –14.86; 95% CI: –32.88 to 3.16, p = 0.11) with high heterogeneity (I2 = 89%), and overall complication rate (OR = 0.66; 95% CI: 0.41–1.04, p = 0.07) with no heterogeneity (I2 = 0%) compared with EA in subjects with OH, as shown in Figures 4 and 5.Due to the lack of available data for certain factors, such as gender, age, and ethnicity, stratified models could not be used to investigate their impact on comparison outcomes. Visual assessment of the funnel plot and quantitative measurements using the Egger regression test revealed no evidence of publication bias (p = 0.87). However, it was shown that the majority of the encompassed RCTs had poor procedural quality, no bias in selective reporting, and only minimal consequence data.
Figure 2
Forest plot of the consequences of wound catheter LAI compared with EA on functional recovery time outcomes in subjects with OH
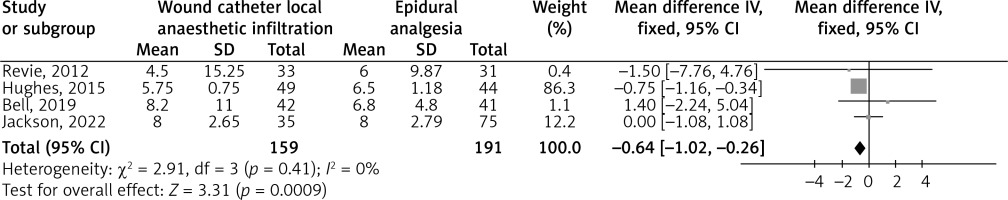
Figure 3
Forest plot of the consequences of wound catheter LAI compared with EA on the incidence of pain score on the second postoperative day outcomes in subjects with OH
Discussion
The current meta-analysis involved 350 subjects with OH at the baseline of the studies; 159 of them were treated with WC LAI, and 191 used EA [7–9, 25]. The use of WC LAI resulted in a significantly lower functional recovery time and higher pain score on the second postoperative day in subjects with OH, compared with EA. However, WC LAI did not show any significant difference in opiate consumption on the second postoperative day and overall complication rate, compared with EA in subjects with OH. This insignificant difference suggests that additional studies are needed to authenticate these findings. The analysis of consequences should be with thoughtfulness due to the low sample size of 3 out of 4 of the designated studies (< 100) and the low number of studies in certain comparisons, e.g. opiate consumption on the second postoperative day and overall complication rate.
Surgical procedures induce a cascade of events, which begins with hypothalamic-pituitary-adrenal axis activation, which in turn releases adrenaline, cortisol, and other compounds that promote inflammation. Preoperative interventions, including anaesthetic administration and some anaesthetic techniques, may influence the postoperative inflammatory response, according to the current body of knowledge [26].
A previous meta-analysis by Li et al. showed that CWI exhibits a higher level of efficacy compared to EA, with a reduced occurrence of problems in surgical procedures. However, EA may offer greater pain management in terms of postoperative pain relief [27]. In addition, Marret et al. have shown that EA results in a notable rise in the occurrence of problems, such as low blood pressure, inability to urinate, and itching, as compared to the use of opioid pain relief administered through injection after colorectal surgery [28]. Also, O’Neill et al. discovered that the occurrence of problems, such as vomiting, nausea, urine retention, and pruritus, is notably greater in the EA group compared to the CWI group following caesarean delivery [29]. However, the current study showed no significant impact regarding complications for both techniques.
A possible explanation for better functional recovery time when using WC LAI is that initial ambulation is more probable in WC subjects due to less postoperative hypotension [9]. EA is well recognised as an active pain control after open abdominal surgery, and it has been recommended in several ERAS guidelines after colorectal and pancreatic surgery [30]. However, a new meta-analysis has recommended that epidurals are not related to quicker recovery after surgery in the setting of ERAS pathways [3], and a recently published ERAS guideline on hepatectomy suggested WCs as a substitute for EA after OH [31]. Concerns have been expressed that WCs might deliver less active pain control in the initial postoperative period than EA after open abdominal surgery, but the existing indication is contradictory [6, 32]. These differences between studies might be due to differences in WC location or restrictions in study strategy. A new meta-analysis of 29 RCTs suggested that preperitoneal catheters are better than subcutaneous catheters and are similar to EA in terms of postoperative pain scores [33]. In subjects experiencing OH via a long upper abdominal incision, the indication that WCs are similar to epidural catheters in pain control is unclear. In an earlier meta-analysis of 705 subjects, pain scores were significantly lower in epidural subjects on the first postoperative day; nevertheless, this did not result in better clinical results, but this study might be subjected to bias because it comprised data from non-randomised studies [32]. Remarkably, pain scores on the second postoperative day were lower in epidural subjects, and this is linked to non-significantly higher opioid intake in epidural subjects on the second postoperative day. This finding suggests that EA might become less active than WCs after the first postoperative day, but the cause for this is indistinct. It can be hypothesised that the decreased effectiveness of EA might have happened because the infusion rate was decreased to offset epidural-associated hypotension, but there are no existing data to support this.
This meta-analysis presented the impact of WC LAI compared with EA in OH. However, additional studies are still needed to exemplify these latent interactions as well as to compare the effect of WC LAI with EA on the consequences studied. These studies should encompass larger more homogeneous samples. This was proposed also in a preceding comparable meta-analysis study, which displayed comparable hopeful consequences of WC LAI in improving the pain score on the second postoperative day and decreasing the functional recovery time [34].
In summary, functional recovery time and higher pain score on the second postoperative day in subjects with OH compared with EA. However, WC LAI did not show any significant difference in opiate consumption on the second postoperative day and overall complication rate, compared with EA in subjects with OH.
Limitations. There may have been some selection bias because several papers found in this study were omitted from the meta-analysis. However, the omitted publications did not adhere to the standards for inclusion in our meta-analysis. Furthermore, we could not ascertain whether age and ethnicity had an impression on the consequences. The purpose of the study is to compare the effects of WC LAI with those of EA in OH. Data from preceding studies were used, which might have led to bias because of missing or incorrect information. The meta-analysis was based on only 4 studies; 3 studies of them were small, i.e. ≤ 100 subjects. The subjects’ nutritional states as well as the characteristics of age, sex, and gender were all potential sources of bias. There may also be some unpublished articles and missing data that could skew the effect being researched. All studies comprised in our meta-analysis were from single-centre organisations and led in the UK, which might border the usage of this data by additional centres, mainly outside the UK, where experimental variations might be affected by differences in clinical practice, healthcare policy, and culture.
Conclusions
WC LAI substantially reduced the functional recovery time and increased the pain score on the second postoperative day in subjects with OH compared with EA. However, WC LAI did not show any significant difference in opiate consumption on the second postoperative day and overall complication rate, compared with EA, in subjects with OH.